Many thanks to Elaine Hunter, National Allied Health Professions Consultant with Alzheimer Scotland for this blog
Background
Connecting People, Connecting Support is a new policy document in Scotland and shares how allied health professionals (AHPs) in Scotland can support people with dementia, their families and carers to live positive, fulfilling and independent lives for as long as possible.
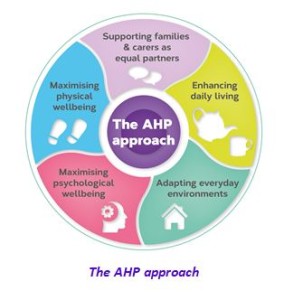
The policy document presents an evidence-informed case to support a biopsychosocial approach to practice for ALL AHPs in Scotland when working with people living with dementia – what we call the AHP approach. The fundamental understanding driving the AHP approach is that people living with dementia CAN benefit from AHP-led interventions. In this week’s blog we are sharing the AHP contribution to maximising psychological wellbeing.
Maximising Psychological Wellbeing
What do we mean by psychological wellbeing?
The central importance of finding ways to communicate (verbal and non-verbal) that work for each individual and which make meaningful connections that may have wide-ranging benefits in relation to overall wellbeing and quality of life is recognised. Psychological interventions of different intensities are reflected to promote emotional health and psychological wellbeing, with the provision of psychological interventions for depression, anxiety, and expressions of stress and distress. This element builds on established AHP psychological interventions and therapies.
Why is psychological wellbeing important?
People with most types of dementia will at times struggle to find the right words or follow a conversation.
- Communication difficulty can be exhausting for the person, families and carers
- We know that people can often find it difficult to talk about dementia and many people living with dementia experience social isolation
- Dementia can have a profound psychological impact and may be linked to feelings of anxiety and depression.
- A non-pharmacological therapeutic approach is advocated for the treatment of psychological symptoms and a person-centred stepped-care model of support.
3 ways allied health professionals CAN maximise psychological wellbeing?
1. Maintain and maximise communication
AHPs are aware that optimum communication occurs in environments that are comfortable, where a person can feel relaxed and safe, and when the AHP-led intervention is tailored and individualised. AHPs have experience in training others in conversation skills and cuing strategies, identifying key elements for effective everyday communication and supporting opportunities to practice communication strategies in a social context, helping the person to gain confidence in the interaction. Speech and language therapists can provide personalised communication advice (aimed at, for example, developing communication passports, assessing communication networks and maximising communication opportunities) that is shared with family members to facilitate their communication skills. Where language difficulties present as a primary feature of the dementia, as in primary progressive aphasia, speech and language therapists will carry out assessments to identify specific communication impairments and abilities. Their findings will contribute to the diagnosis and be used to plan therapy and strategies.
2. Psychological interventions
AHP core psychological skills are unique to each profession and vary according to their undergraduate education and postgraduate development activity. AHP interventions to maximise psychological wellbeing require excellent communication skills and the ability to integrate psychological interventions and psychological therapies into core AHP practice. A number of approaches based on the psychological understanding of dementia and its effects, including reminiscence approaches, life-story work, anxiety management, and engaging in everyday occupations and activities, will be core to AHPs’ day-to-day practice.
With additional enhanced training opportunities, psychological interventions can also become core to AHP roles and integral to a team approach to a stepped-care model of assessment and intervention. Psychological interventions include motivational interviewing, behavioural activation, mindfulness based cognitive therapy, cognitive stimulation therapy, cognitive rehabilitation and cognitive behavioural therapy. Specific psychological interventions providing individualised, formulation-led interventions in response to stress and distress in dementia, ranging from low-intensity to specialist interventions, can also be within AHP remits.
3.Psychological therapies
Psychological therapies are highly specialised psychological interventions that include the established AHP disciplines of art psychotherapy and music therapy.
Art psychotherapy creates opportunities for verbal and non-verbal communication by using art to enable people to feel connected to a sense of self, other people and the environment around them. It can support people living with dementia by reducing anxiety and increasing coping skills (Safer & Press, 2011), depending on how interested the person is in art activities, art materials and how they feel about one-to-one or group activities. Art psychotherapy can be particularly helpful for people who find it hard to express their thoughts and feelings verbally, enabling self-expression and enhancing sense of self and personhood.
Music therapy builds on people’s ability to respond to music to develop a therapeutic relationship and facilitate positive changes in emotional wellbeing and communication through engagement in live musical interactions. It has a robust evidence base as an effective, non-pharmacological intervention that can significantly improve and support the mood, alertness and engagement of people with dementia, reduce the use of medication, and help to manage and reduce agitation, isolation, depression and anxiety (Ridder et al., 2013).
These art-based therapies are particularly helpful when people find their emotions are too confusing to express verbally, when verbal communication is difficult or when words are not enough.
Supervision for the AHP professions is integral to all of the interventions.
On reflection
Thank you for taking the time to read this blog and we would like to know
- As an AHP, how do you currently support people living with dementia to maximise the persons psychological wellbeing?
- As person living with dementia, what support would you like to receive from allied health professionals to maximise your psychological wellbeing?
- As family carer, what support would you like to receive from allied health professionals to maximise your psychological wellbeing?
We look forward to hearing from you.
Email me at EHunter@Alzscot.org
References
There are references supporting this text which you will find in the original policy document and can be viewed here https://www.alzscot.org/assets/0002/7356/AHP_Report_2017_WEB.pdf with all the evidence informing the policy available at www.alzscot.org/ahp
On the 17th April we held a seminar exploring the innovative work being done to support young people with communication needs within justice and mental health settings in both New Zealand and Scotland Read about the morning in our first blog Talking Trouble, New Zealand kindly gave a gift to all delegates of their fantastic Top Tip cards shown in the photo . You can download your own set here
The afternoon session continued the underlying theme that communication support needs are often hidden and many looked after children have support needs that remain unidentified.
Dr Ann Clark from Queen Margaret University presented her research findings looking at Panel members’ and Children’s Reporters’ perspectives on communication in Hearings. Her informative presentation highlighted the need and desire for more training on Speech, Language and Communication Needs. The conclusion was that it is better to assume ALL children who are attending a Hearing have additional support needs, whether or not they have a diagnosis of Speech Language and Communication Needs (SLCN) and Social Work support is also essential in achieving positive outcomes for Looked After Children. SLCN in Hearings April 2018
Our interactive session asked participants to reflect on the information presented during the day and to think about opportunities to improve practice in supporting communication as well as the barriers faced. The main themes that emerged from the barriers were:
- Identifying Speech, Language and Communication Needs in children and young people
- Constraints within Speech and Language therapy services
- Lack of education and training – the word “communication” because practitioners think they know about it when in fact there is a large knowledge gap
- Routes to services can be either Offending or Mental Health pathway
- The balance of power and control in relationships between the practitioner and the person with SLCNs – how committed are we to put genuine inclusive communication approaches in place.
Identify the barriers helps to inform the opportunities and the themes emerging were:
- Some good collaborative practice is happening already and the impact of working together is proven in research – we need to extend this further.
- Joint training sessions – good visual and other communication supports
- SLT have a vital role going forward
- We have a real opportunity at the moment to effect real change in a legislative context with recent Government policy
Kim Harley Kean, Head of the Royal College of Speech and language therapy Scotland office concluded the day and injected a great sense of impetus going forward. She asked 2 key questions:
Q: Is communication support and equality an issue in justice and care services?
Q: Do we want to do something about that?
Having responded with a unanimous YES she helped us to see the potential we have for change. It was obvious from the day that collaboration is vital and the event demonstrated how many different professions and organisations want to do something about the issues. We can be more effective if we do this collectively, even across continents!
The majority of participants felt we should use the event to establish a collaborative network. The key purposes would be to:
- Market – get message out there – tell more people – politicians, government and public – about Speech Language and Communication in Criminal Justice Settings explaining how SLT and Talking Mats have a vital role.
- Share stories, gather evidence.
- Facilitate enriching conversations between practitioners, for example, about aptitudes and approaches needed to negotiate communication behaviour change among professionals as well as people with SLCN…
If you would like to join the network and help to influence change please email info@talkingmats.com with a request to add your name to the youth justice mailing list.
Addressing the communication needs of people in youth justice is key to improving lives. The lack of attention to this is costly. On the 17th of April, we organised a seminar to look at the underlying issues and share good practice.
We were delighted with the collaborative mix of people attending. We had representatives from: the Scottish government, the NHS; Third sector organisations working in youth justice, the police, social workers, professional bodies, universities and social work.
Our thanks to Professor Richard Simpson for chairing the day and setting the tone by emphasising from the start that understanding communication is key to improving service delivery. Following his introduction a series of excellent and stimulating presentations took place creating a fusion of ideas and practice from Scotland and New Zealand.
- Kim Hartley Kean, head of the Royal College of Speech and language therapy Scotland office highlighted the current position in Scotland
- Sally Kedge and Alayne Mckee described the approach adopted by their organisation Talking Trouble in New Zealand.
- Jane Macer the therapeutic service co-ordinator from Starley Hall Fife described an whole system approach to embedding good communication practice within an organisation
- Yvonne McKeown and Sandra Polding Speech and Language Therapists working with young people in a NHS inpatient psychiatric unit in Glasgow shared some case examples.
In different ways the speakers brought up very similar themes:
- Communication can be treated glibly. There is a lack of understanding of what communication difficulties are and of the impact that they have on the lives of young people. These difficulties are often hidden and take time to identify. Lack of identification can have a huge impact on the future lives of young people.
- Finding ways to hear the young person’s voice is key both for the young person but also for organisations in order to deliver appropriate and effective care.
- Recognition of the intergenerational cycle and the importance of getting care and support correct so we break patterns and enable change.
- Providing collaborative solutions and understanding the breadth of communication will help services improve. However, given services often don’t know what they don’t know in terms of the impact of communication difficulties we have to find ways to express those solutions in language that those services can relate to and understand. Listening to organisations and exploring their processes by analysing the communicative demands of each stage can be a helpful way to start.
- Moving forward it is important to knock on open doors i.e. work with people who are receptive to recognising the impact of communication difficulties on young people and their lives but also find the strategic influencers who are sympathetic, in the words of our New Zealand colleagues ‘the aunts and uncles in the field’ who can help to promote the issue and raise awareness at a National level.
- You can’t explore the issue of trauma and adverse childhood experiences without certain precursor, building blocks being in place. This takes time and requires a constancy of approach.
- The importance of inclusive, visual tools becoming common place so that they are not used in isolation and in a vacuum.
- The challenge of supporting and nurturing a young person’s inner voice when they have significant difficulties with language.
- Lack of understanding of communication difficulties may lead to services responding to internalized behaviours that can lead to a fork in life; one way can send the young person down a route of offending behaviour services and the other mental health services.
- The solutions lie in partnership and collaboration between professions and services.
There were lots of creative ways of using Talking Mats that were shared. A couple of examples that stand out were
- Using Talking Mats with social workers to help them unpick what they already know about a young person’s language and communication. This approach helped them think about all the different aspects that contribute to communication and where the young person’s strengths and weaknesses lay e.g. non verbal communication , humour , word finding , understanding complex information, understanding simple information etc .
- Using Talking Mats to support a psychiatric assessment of a young person. One person used his Talking Mat to say he was hearing voices something he was unable to disclose verbally. In this case this enabled an accurate mental state assessment and non-custodial sentence.
I will leave the last word to a young man living in an inpatient unit to support his mental health, his words about communication difficulties are ‘They make you more vulnerable when bad stuff happens’ how true that is and this is why it is important we work together to improve services .
Next steps The community justice network met in the afternoon and were challenged to think about the opportunities and barriers in developing services – read the for blog that covers the afternoon ……… If you missed the seminar and want to join a multiagency network to discuss this and help take this forward in Scotland then please let us know .
Click to read the excellent presentations from the seminar
- CJSCENTalkMatsPresentation170418
- Talking Mats presentation 17 April 2018 Sally Kedge Alayne McKee TTANZ final
- TM seminar 04-18
- Talking Mats & Justice CEN April 2018 Draft
Talking Mats in Germany is being extended by one of our trainers Professor Norina Lauer. Here she describes two of her current interesting projects and we look forward to reading her findings.
The German version of the Talking Mats app will now be tested in two more projects in the west of Germany. As the communication symbols were developed for English-speaking clients six German SLT students of the Hogeschool van Arnhem en Nijmegen (han) in the Netherlands want to find out if the words and symbols fit to German clients and their cultural background. Because of cultural differences between Scotland and Germany it is necessary not only to adapt the language but also check the icons.
One of the projects will be conducted with children between the ages of 8 and 10 years. The children will be asked to classify the symbols from their age-group. The question will be whether the symbols and words are relevant for the situation of German children. If not, they will be asked for possible alternatives.
The other project focuses on adults. One group of people with aphasia and one group of healthy persons will be tested. Every tested person scores the 57 icons concerning their correspondence with the words written down below by using a scale from 0 to 3. In addition, possible graphic alternatives will be enquired and collected. The two groups of adults will be used to determine if there is a significant difference between the obtained results from each group.
Our next train the trainer course is in 2 weeks and we’re looking forward to welcoming people from a range of professions and a range of places- New Zealand, Japan, England and Fife!
Becoming a trainer for Talking Mats means the staff member can offer Foundation training within their organisation or partnership. This ensures that the standard of the communication and thinking tool is maintained and sustainability of its use is supported. It is a positive investment for organisations in person -centred practise.
The trainers are provided with resources for delivering the Foundation course and their licence is renewed annually .
Comments from people who attend include:
Practical approach to training made it easy to try out and learn from ‘doing’
A wonderful inspiring course- really looking forward to continuing to work as part of the TM team
Really enjoyed the training. Learnt a lot not just about my use of TM but also just about myself as a presenter and communication
If you’ve attended a Foundation course and would like to become a trainer, our next course is in June. You can find out more details on our webiste or on this link 20180621 Accredited Training flier Jun 2018
Apart from the necessity of fulfilling the requirements of the General Data Protection Regulation which has to be completed by 25th May, I have been pondering on other advantages of complying with the GDPR.
Here at Talking Mats we are all going through files, bagging up paper for shredding, deleting data files on our master computer and preparing text to send to all our customers and contacts to make sure we only hold information that is adequate and relevant.The first advantage for us is that it’s a good way to re-establish contact with people.
I’ve been given the task of going through all the research data and have ploughed through 16 drawers of research data starting in 1992! Way back then I worked with a wonderful professor who was keen to hold onto all our raw data just in case we wanted to check or replicate anything. Its all been under lock and key but the time has come to bite the bullet and get rid of it. I found this to be not only nostalgic but also emotional – all those fantastic participants who gave us their time and insights.
Its also been cathartic because as well as filling bags for shredding I am smashing up discs of video footage. We filmed lots of people with a range of communication difficulties using Talking Mats to compare with the same conversations without Talking Mats to analyse any differences. So… another big advantage is that I’ve destroyed all evidence of my dodgy hair cuts throughout the years!!
I counted 41 completed projects going from the very first one in 1992 which was a demographic survey of people who used AAC (Augmentative and Alternative Communication) systems in Scotland. In 1998 the Gannochy Trust funded the original project where Talking Mats was born Gannoch Final report. We then went on to carry out a wide range of projects which include working with people with Motor Neuron Disease, Stroke, Learning Disability, Children with Additional Support Needs, people living with Dementia to name but a few. The website contains the final reports on all our projects and in looking back at them I am also very proud of the good quality research the team here at Talking Mats has carried out.
Many others are now doing projects using Talking Mats but I leave it to them to organise their own GDPR and hope they also find the process worthwhile and rewarding and not just seen as a chore to be done.
‘For every pound invested in the Talking Mats Keeping Safe resource and training there is a potential saving to services of £23.00’ .This was the findings of a cost benefit analysis carried out during the development phase of the Keeping Safe Talking Mat resource. A Cost-benefit analysis demonstrates the overall economic value of an intervention with numbers and evidence.
The Keeping Safe resource
The Keeping Safe resource is a visual framework that has been developed and trialled over 6 years in partnership and with funding from various organisations e.g. Survivor Scotland, Scottish government , Kingdome Abuse survivors project and NHS Fife
The Keeping Safe resource provides:
- A listening space for people with learning disability and communication difficulties to raise concerns and express their point of view.
- A structure for staff to find out what people are thinking about their lives, and raise issues that can be difficult to discuss.
A reflective practice training was developed and provided to over 700 staff to allow staff become familiar and confident with using the the resource
Findings of the cost benefit intervention
There is a significant financial advantage to services using Talking Mats. Analysis of six scenarios found that for each pound invested in the Keeping Safe training there is a potential saving to public services of £23.00. In learning disability services it is easy for costs to accelerate quickly. If services don’t respond effectively, challenging behaviours can escalate and relationships and placements are at increased risk of breakdown. Talking Mats can help provide staff with a comprehensive and accessible framework to help them listen to people who can find it difficult to articulate what is really going on for them e.g. issues of pain, relationships or levels of support. In this project 89% of Talking Mats resulted in staff learning new information about the person they were working with, even when they thought they knew them well. The Talking Mats framework provides a way to turn these points of views into actions that can be monitored and reviewed. It is these early interventions that not only save money but improve quality of life.
Cost benefit Process
With support from Inspiring Scotland a cost benefit analysis was done that examined the cost of the Talking Mats intervention and any resulting actions. 6 cases were chosen from over 100 detailed descriptions of how practitioners working with people with learning disabilities had used the resource. These descriptions represented a cross spectrum of people with learning disabilities in Scotland in terms of living situations e.g. living at home , in supported settings and an inpatients facility . They were also chosen to represent the comorbid conditions that often exist with learning disability e.g. autism, mental health and cerebral palsy. An alternative scenario was created and tested with critical friends as to the likelihood of what might have happened without the Talking Mats intervention. All the scenarios that were developed are available here 20180110 scenarios cost benefit The primary source of financial information and the subsequent calculations was the Unit Costs of Health and Social Care produced by the Personal Social Services Research Unit (PSSRU) 2015/16 . This contains detailed cost estimates for a range of services such as care placements, NHS services, social work, mental health, and family interventions. This analysis can only be illustrative as assumptions are subjective.
The findings from our final report 160512 Keeping Safe report 2013-2016 showed that effective use of the resource not only led to improvements to quality of life for individuals but that it can save services money. Book a place on our webinar and get the Keeping Safe resource 20180122 Keeping Safe Webinar or if face to face discussion is more your thing attend the advanced course in April 2018 – you get the resource with that booking too!
This new resource has been developed by Strathcarron Hospice and Talking Mats to help people with advanced illness or long term conditions to think ahead and plan for the future.
It consists of a booklet and 3 topic symbol sets: Affairs; Care/treatment; Personal values
It can be used to help people have conversations about:
• the extent to which their personal affairs are sorted;
• what they would or would not consider about future treatments and care;
• what is going well/not going well in relation to their personal values
It is widely recognised that having discussions about end of life issues can enable people to remain in control for longer and help them to identify the care and support they need and want as they approach death. In spite of this, in Scotland:
- 74% of people have not discussed what their wishes would be if they did not have long to live
- 79% of people don’t have any written plans for their end of life care, financial wishes or funeral plans
- Only 35% of people have written a Will
It can sometimes be difficult for people to start conversations about planning for end of life and people this is exacerbated if people have specific difficulties communicating their thoughts and feelings because of symptoms, fatigue and emotional factors. Before initiating this type of conversation it can be helpful to check the extent of a person’s understanding of their illness and whether or not they want to talk about the future.
The importance of having conversations and making plans for end of life has been highlighted as being relevant for people in the early stages of life limiting illness as well as for those nearing the end of life. There is evidence that people who have Advance or Anticipatory Care Plans in place are more likely to receive the care that they want and treatment can be less invasive. ACP is a process rather than a one-off conversation. It is acknowledged that ACP discussions should take place in appropriate settings with sufficient time to enable to people to consider and weigh up different options. ACP should also be developed in line with peoples’ personal values and goals (Sinuff Tasnim, et al.(2015) “Improving end-of-life communication and decision making: the development of a conceptual framework and quality indicators.” Journal of pain and symptom management 49.6 2015): 1070-1080).
Perhaps we should think about planning ahead whether or not we have advanced illness or long term conditions??
Training
To get the most out of the resource we run half day advanced training courses which will include the Thinking Ahead Resource. This course will be relevant to you if you:
- have attended a Talking Mats foundation training and are experienced in using Talking Mats with adults
- want to extend your use of Talking Mats and consider its role and application to advance care planning
- want to discuss sensitive topics around end of life care
Please contact us at 01786 479511 if you are interested in future dates.
Do you want to introduce Talking Mats to people with a communication disability and autism, but know they will need support to learn it?
We are holding a 2 hour seminar on the 1st of February in Stirling to share ways of supporting people with autism to learn to use Talking Mats and express their thoughts.Twilight ASD Seminar
Do you want to help people think about the future and what they might want to have in place at end of life? Talking Mats and Strathcarron Hospice have developed a powerful new resource to support these sensitive conversations and an advanced course is being held in Stirling on the 21st February and in London 27th of March http://www.talkingmats.com/training/specialist-seminars/
These opportunities are only open to people who have attended Foundation training
Sally Kedge, Speech and Language Therapist from Trouble Talking New Zealand shares two powerful case examples of using Talking Mats with children and families caught up in the criminal justice system.
This week it was hot in New Zealand, so I sat under a tree in a school playground in the shade with an eight-year-old girl to do a Talking Mat. I’m a speech-language therapist engaged by the child protection agency who have guardianship of her. This doesn’t happen that often in NZ but the team involved with this girl and her brother realised that as well as dissociative behaviour related to the impact of trauma due to family violence exposure, there was also significant difficulty with language acquisition for both children. The mix of a trauma history and a language disorder was resulting in significant difficulty expressing emotions and explaining what had happened when behavioural outbursts happened.
Some of my work with this child has been to help the team understand how her language profiles impacts on her life, and to develop her language skills at school via a programme she carries out with a teacher-aide and a friend. My role has also involved helping her understand her own life story and to equip her to process this, as it hasn’t been a pretty ride so far.
At a multidisciplinary planning meeting for her and her sibling recently, the team were concerned to make sure the children had accurate information about when their father was going to be released from prison. Their mother has recently been released too but no one knows where she is currently. I suggested a Talking Mat might help us to find out what she knows at the moment about her parents and how she felt about the next few months, as there are likely to be some changes happening in her world. We wanted to give her accurate information so she didn’t need to fill in the gaps herself.
Using a Talking Mat helped me establish that currently this child feels many things in life are going well. This is good progress. However, we identified a few things that she felt were not going that well at school (‘in the middle’) and I was then able to talk to her teachers about preparing for the new school year starting in February. We figured out that she is looking forward to seeing her dad but doesn’t know when she will see him or where he is going. A conversation with her Social Worker and the drug rehabilitation residence has allowed me to put together some visuals and a timetable to show what is going to happen next. Dad can have these as well as her carer and others in her team.
Another child with a similar history also did a Talking Mat with me last week. My purpose was to help the team find out how he feels his current care situation is going. A very mixed picture emerged with some concerning cards placed in ‘not going well’. I asked the boy at the end if he knew anyone who could help him with those things and he said, ‘no one’. I was able to explain that I am one of the adults who need to figure out how to make life easier for him and I would talk to some other adults and come back to see him. The photo I took of the Talking Mat allowed me to follow up with the team and I took the photo back to the boy to explore further some of the ‘not going well’ cards. At this second visit, this boy initially did not want to speak at all, but he engaged fully in looking at the photo of the Talking Mat with me.
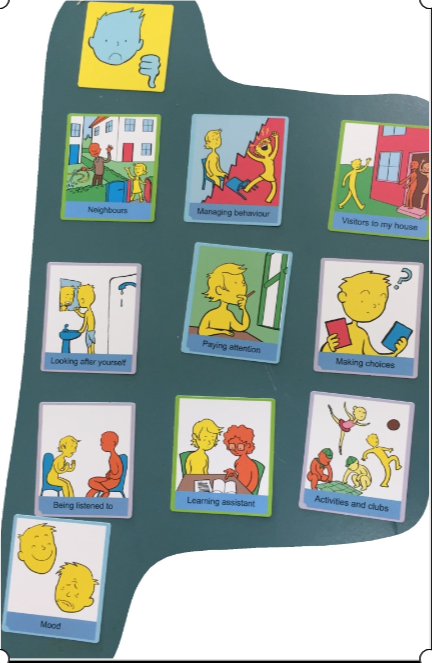
We used a scale of 1 – 5 (how much of a problem is this for you – 1 = not much, = 5 = really really bad) on a piece of paper that he could mark with a pen to explore the ‘not going well’ items in the photo. He picked out ‘mood’, ‘people coming to his house’ and ‘learning at school’ as ‘really really bad’. We agreed that these needed to get sorted out for him to make life easier and we agreed who I could talk to about these things. Once we got that agreed and written down, he initiated some conversation about less heavy topics and started playing. I’m now following up with the team. Easier said than done, but without the Talking Mat I don’t think we would have got his views so clearly.
Our Talking Trouble Aotearoa NZ team is involved with children, young people and adults involved with care and protection, justice, mental health and behaviour agencies. We have been very excited about the wide range of opportunities that Talking Mats has provided us and the professionals we work with to explore people’s views on their own situations, their preferences, and their well-being. This year we’ve been exploring how Talking Mats might be used in our contexts:
– in sexual assault health assessments undertaken by specialised health professionals
– for Social Workers in our Youth Justice and Care and Protection Communication Projects
– When finding out about how people feel about talking and understanding in legal contexts such as courts and Family Group Conferences when we are engaged as court-appointed Communication Assistants (equivalent to ‘intermediaries’),
– and in our own speech-language therapy assessments and interventions.
The social workers, paediatricians, teachers, lawyers and others we work with have also been excited about exploring how Talking Mats can assist in these contexts. We’re looking forward to more training from the Talking Mats team next year.
sallykedge@talkingtroublenz.org
Come and hear Sally speak at our Criminal Justice Seminar on the 17th of April 2018. Contact info@talkingmats.com for more information.
 Online training login
Online training login