Talking Mats is delighted to welcome a new Training Associate, Jess Lane. Jess has written this blog to introduce herself to the Talking Mats community. Welcome, Jess, we’re thrilled to have you as part of team TM!
Hello! My name is Jess and I am thrilled to be introducing myself as a newly appointed Training Associate for Talking Mats.
About Me
I am a Specialist Speech and Language Therapist with a clinical background in Learning Disabilities and Paediatric Mental Health. I also work for the Royal College of Speech and Language Therapists (RCSLT) as a Research and Outcomes Officer, where I help to build research capacity, capability and culture within the profession. I am currently studying towards a Clinical Doctorate in Professional Health Studies, looking at the use of Talking Mats for facilitating the direct and meaningful involvement of children in care planning.
Talking Mats has been a huge part of my career to date. This began in my hometown of Gloucester, where I worked as an SLT in an Intensive Support Service for children and adults with learning disabilities. Changes in my personal circumstances saw me relocate to Scotland in 2022, where I worked across Specialist Child and Adolescent Mental Health (CAMHS) Services in and around Glasgow. Most recently, I worked at a National Child Inpatient Psychiatric Unit (CIPU), supporting children with severe and enduring mental illnesses.
Talking Mats in CAMHS
Since completing my Licenced Training last year, I have been working with Talking Mats to deliver Foundation Training for CAMHS teams across the UK, as well as driving an upskilling initiative for Specialist Children’s Services locally in Glasgow. I have found that Talking Mats provides children with a safe space to explore topics that they might otherwise feel unable to communicate about, in a way that is highly supportive, sensitive and impactful. This is encompassed by feedback from a recent patient, who wanted to share that “using a Talking Mat is easier than talking because talking about how you feel can be difficult”.
Many of the children admitted to CIPU present with transient communication difficulties that can exacerbate the impact of mental ill health. Some children present with underlying communication difficulties that were not apparent in the community setting. Other children do not present with communication difficulties, but find it extremely difficult to think about, or share their views on, sensitive topics. Because of this, Talking Mats have been used extensively by the multidisciplinary team on CIPU to:
- Facilitate the direct involvement of patients in goal setting and care planning
- Adapt and extend traditional mental health inventions, including talking therapies
- Support capacity assessments, assessments of mental state and medication reviews
- Improve engagement with local advocacy services as part of the CTO process
- Adapt and extend assessments such as the Child Occupational Self-Assessment Tool
- Improve access to psychoeducation for patients with anxiety and/or depression
- Improve engagement with meal planning for patients with an eating disorder
- Support the differential diagnosis process for mental illnesses such as catatonia

Using Talking Mats in an acute mental health setting has transformed the way clinicians from across Nursing, Psychiatry, Dietetics, Occupational Therapy, Physiotherapy and Psychology engage with the children about their care and treatment. Feedback from the clinical team, children and their parents/carers has been overwhelmingly positive. Talking Mats are now used routinely on the unit to support children’s access to (and engagement with) therapeutic intervention as part of their wider recovery, as well as ahead of all multidisciplinary team meetings and case conferences to ensure each child’s voice is heard and acted upon.
I am so pleased to have joined the Talking Mats team and am very much looking forward to supporting other people to use Talking Mats in a range of settings. Stay tuned for a follow up blog on how I have used Talking Mats as part of a post-diagnostic package of support for autistic children and young people, designed to support more focussed, strengths-based conversations around what it means to be autistic, in line with the core principles of neurodiversity affirming practice.
This year’s campaign focuses on the importance of all children and young people whoever they are, and wherever they are in the world, to be able to say – and believe – “My Voice Matters.” Talking Mats is a tool that allows the voice of the young person to be heard. Read these blogs on Mental Health and Young People to find out more.
- Dr Carla Innes, Clinical Psychologist for Learning Disabilities at Stockport Healthy Young Minds (CAMHS) describes how Talking Mats helps the team to gain more insight to the children and young people they are working with, and how it has helped intervention focus on the child’s potential, and zone of proximal development.
- This work in Stockport is further expanded on in a presentation by Dr Rosie Noyce, Clinical Psychologist, given at the Talking Mats 21st Birthday Event in August 2019.
- Sally Kedge, SLT with Talking Trouble, New Zealand shares 2 powerful case examples of using Talking Mats with children and families caught up in the Criminal Justice System and demonstrates how the connection with a therapist can be the key to unlocking feelings and emotions
- Natalie Paris, Project Lead for Cashback180 programme based within Mayfield and Easthouses Youth 2000 Project, shares stories of using Talking Mats with young people in Midlothian.
- Our Director, Margo MacKay, describes using Talking Mats to ask young people about their environment and the impact different environments can have on wellbeing.
- Laura Holmes, our Lead Associate for Children and Young People, writes about the Virtual Schools Team in Wigan and how they used Talking Mats with Looked After Children.
To find out more about Talking Mats Foundation Training for you or your organisation, click here.
In the first of 2 blogs on Selective Mutism, Vanessa Lloyd of Birmingham Women’s and Children’s NHS FT describes using Talking Mats to give a young boy the opportunity to communicate at a time when talking was too hard.
Using Talking Mats with a primary school aged child with developmental Selective Mutism
Selective Mutism is a form of social anxiety characterised by stark differences in how a person communicates in different situations. There is also acute awareness of everyone around them who may be listening, either intentionally or accidentally. In Education settings Selective Mutism often become apparent at times of transition and teachers often describe a very different child to the one a parent knows at home. As a school therapist I have the job of finding the puzzle pieces and bringing them together in a way that home and school can understand. I have found the Talking Mats approach to be very useful when working in this area. Here’s an example;
I recently took a referral for ‘A’ who is 6 years old:
Main points from school:
- Joined 12months ago
- Not spoken at school in those 12 months
- Staff felt they didn’t know him
- Staff assumed he was happy not joining in
Main points from parents:
- Aware he is quiet in school
- This is who he is and he has been like this since starting Nursery
My observations indicated Selective Mutism;
- his body language indicated anxiety in situations where he was expected to speak or interact
I needed a way to feedback this anxiety to staff and for A to be heard without using his voice. After building a rapport with him I introduced Talking Mats and offered him the opportunity to engage
Getting Started
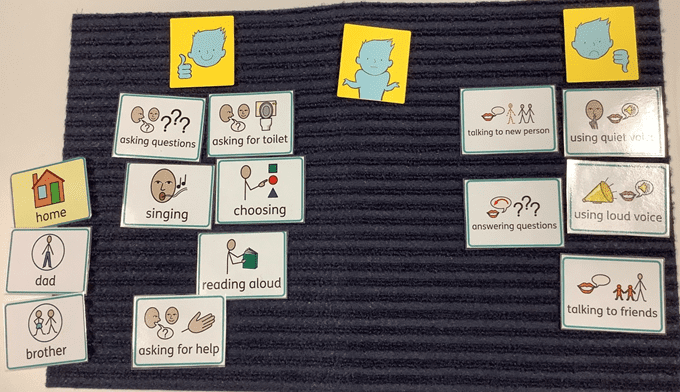
Using the Primary Communication Rating Scale (Johnson & Wintgens, 2016) as a basis, combined with an image system he was familiar with, I planned the symbols needed to support the conversation and set out the expectations for the activity. Fundamentally, I made it clear that he did not have to talk to me to participate.
How it went
The school environment.

As anticipated, he made his feelings instantly clear about the activities where he was required to talk, rapidly sorting them into ‘unsure’ or ‘don’t like’.
What was less expected was how relaxed his body language became, particularly when I suggested showing his class teacher. It was as though he knew that there was some power behind his arrangement of these symbols and he was ready to embrace it.
Follow up
Talking at home.
Having fully grasped the potential of the task, this young boy set to work answering my questions through careful consideration and placement of symbols. The same questions that would otherwise spiral him into a freeze or flee response were now being answered with a newfound command of the situation. He had things to say, things he wanted people to know, and in that moment, he had a way of doing this
Taking it forward:
Showing the child’s perspective provided a powerful way of highlighting to school the misguided assumptions that had been made about his feelings and attitudes towards talking. The Talking Mat conversations opened the discussion about the importance of Selective Mutism intervention and created a platform for the child to be involved and be heard. He was a valued contributor in an environment which was previously inaccessible for him.
We are all continuing to live in challenging times due to the COVID-19 pandemic, and there are concerns about the impact on the mental health of people at all ages and stages of life. This is a good time to reflect on the wide variety of blogs that have signposted how useful Talking Mats can be in helping people to think, structure coherent responses, and express their views. If this is an area of interest to you then take a look at these blogs to find out more:
- Debbie Mole, Clinical Nurse Consultant in Mental Health and Intellectual Disability for DHM Mental Health Care in Melbourne, Australia shares a great example of the positive impact Talking Mats can have for people who have experienced trauma. https://www.talkingmats.com/talking-mats-and-trauma-work/
- Natalie Paris, CashBack 180 Project Lead shares some powerful examples of how Talking Mats has helped her to open up conversations with the young people she works with https://www.talkingmats.com/opening-up-conversations-with-young-people/
- Edith Barrowcliffe from The Action Group demonstrates how Talking Mats has allowed individuals with intellectual disabilities access talking therapies and counselling. https://www.talkingmats.com/counselling-communication-1/
- Edith expands on this work in her second blog, describing how she adapted this approach to use during remote support during lockdown. https://www.talkingmats.com/counselling-learning-in-lockdown/
- Jo Brackley, NHS Clinical Lead for SLT Secure Services (Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust) describes how Talking Mats helps people with mental health open up and have richer conversations, with increased novel information gained. https://www.talkingmats.com/covid19_securehospitalsetting/
- Susan Gowland, SLT at NHS Fife Forensic Learning Disability Service, describes how Talking Mats support patients to express what they think in forensic learning disability setting. https://www.talkingmats.com/forensic_ld_setting/
- Dr Carla Innes, Clinical Psychologist for Learning Disabilities at Stockport Healthy Young Minds (CAMHS) describes how Talking Mats helps the team to gain more insight to the children and young people they are working with, and how it has helped intervention focus on the child’s potential, and zone of proximal development. https://www.talkingmats.com/talking-mats-and-mental-health/. This work in Stockport is further expanded on in a presentation by Dr Rosie Noyce, Clinical Psychologist, given at the Talking Mats 21st Birthday Event in August 2019. https://www.talkingmats.com/wp-content/uploads/2019/08/Talking-Mats-and-Young-Peoples-Mental-Health.pdf
- Georgia Bowker-Brady, Advanced Specialist SLT (Berkshire Healthcare Foundation Trust) describes how using Talking Mats in dementia care and acute health patient inpatient services helps patients organise their thoughts and express what is going well for them, as well as what isn’t. https://www.talkingmats.com/acute-mental-health/
- Rachel Woolcomb, Talking Mats OT Associate, explains why Talking Mats supports thinking, and why it can be particularly useful in helping people to structure and express their thoughts. https://www.talkingmats.com/talking-mats-as-a-thinking-tool/
We would love someone to carry out some research in this field, so if this sparks a research or blog idea, please get in touch with us at info@talkingmats.com.
The Talking Mats Foundation Training is a course that builds people’s confidence in using and applying Talking Mats to their work. Organisations can access this as a group ensuring staff can embed the Talking Mats approach and principles into their practice. The training also gives staff a common language for embedding a patient centred approach at the heart of a service.
We offer online training by;
- giving organisations access to our online training platform – this is designed as self-directed course, supported by a Talking Mats tutor, with a variety of activities and resources to support learning
- zoom/teams sessions
- a combination of both 1 and 2.
2020 saw an increase in organisations approaching Talking Mats for online team training and this has continued into 2021. We will work with you to find the approach that best suits your staff group.
Online learning does not suit everyone and comments from participants are mixed. Some really like the flexibility of being able to work at their own pace and find the site user friendly whilst others miss the interaction that face-to-face brings. As a team we miss the face-to-face training too but believe that our online training and the support we offer organisations is an excellent alternative.
It is easier to discuss the impact of an organisational course by giving an example. We recently ran a course using our online learning platform combined with short introductory and a follow-up session on Zoom for 24 staff working in an NHS Paediatric service. Taking part on the course were Nurses, Psychologists, Occupational Therapists, Physiotherapists, Dieticians and Speech and Language Therapists. It was great working with such a multidisciplinary group. They all have communication at the heart of their practice and were keen to learn about a framework that could help them improve the effectiveness of their work. There were different reasons for doing the course, but a common theme was wanting to have more ways of directly engaging and building relationships with the children they were working with rather than relying mostly on carer views. They wanted to be able to involve young people more meaningfully in some of the complex issues that surrounded their care.
It is always positive when a course has immediate impact and this staff group applied their learning in very different ways, for example Talking Mats was used to;
- communicate with a young person with selective mutism,
- involve a young woman who was self-harming to contribute to the strategies that help her reduce those behaviours ,
- involve children in physiotherapy interventions.
One course participant said ‘I have practised with a couple of patients and it has made a massive impact on their lives already. One patient’s behaviours have dramatically reduced as I was able to support her to show how she felt about aspects of her care and resolve this.’ And another participant said ‘I have now used Talking Mats with a couple of young people with complex neurodevelopmental difficulties and this has helped engagement considerably, where things had felt stuck before’
An important part of Talking Mats training is to help participants think about their own communication style and how it impacts on interactions and relationships. Staff said;
- this course increased my awareness of my communication style and made me reflect more on how I communicate with my patients but also what I presume from my patients.
- I am more aware of the communication demands I place on others as a clinician/therapist and am more confident in engaging people with communication difficulties.
- It has made me think more about the language that i use during interactions.
- It has definitely made me reflect on my own style of questioning, and helped improve my pacing and language skills.
The feedback from this varied and engaged group of staff was positive and is summed up in this comment; ‘The course was very engaging, interesting, and easy to follow and understand. I have learned a lot from this. The reflective work throughout the modules really helped to connect the theory with the practice of Talking Mats. The course leaders were very involved, supportive and helpful!’
Our training is relevant to organisations working within Social Work, Advocacy, Dementia Support and Education as well as Health and Social Care. If you think you would like to organise a course for your staff group please get in touch at info@talkingmats.com to talk it through.
In the UK we are emerging out of lockdown and there are concerns about the impact on the mental health of people at all ages and stages of life. This is a good time to reflect on the wide variety of blogs that have signposted how useful Talking Mats can be in helping people to think, structure coherent responses, and express their views. If this is an area of interest to you then take a look at these blogs to find out more:
- Edith Barrowcliffe from The Action Group demonstrates how Talking Mats has allowed individuals with intellectual disabilities access talking therapies and counselling. https://www.talkingmats.com/counselling-communication-1/
- Edith expands on this work in her second blog, describing how she adapted this approach to use during remote support during lockdown. https://www.talkingmats.com/counselling-learning-in-lockdown/
- Jo Brackley, NHS Clinical Lead for SLT Secure Services (Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust) describes how Talking Mats helps people with mental health open up and have richer conversations, with increased novel information gained. https://www.talkingmats.com/covid19_securehospitalsetting/
- Susan Gowland, SLT at NHS Fife Forensic Learning Disability Service, describes how Talking Mats support patients to express what they think in forensic learning disability setting. https://www.talkingmats.com/forensic_ld_setting/
- Dr Carla Innes, Clinical Psychologist for Learning Disabilities at Stockport Healthy Young Minds (CAMHS) describes how Talking Mats helps the team to gain more insight to the children and young people they are working with, and how it has helped intervention focus on the child’s potential, and zone of proximal development. https://www.talkingmats.com/talking-mats-and-mental-health/. This work in Stockport is further expanded on in a presentation by Dr Rosie Noyce, Clinical Psychologist, given at the Talking Mats 21st Birthday Event in August 2019. https://www.talkingmats.com/wp-content/uploads/2019/08/Talking-Mats-and-Young-Peoples-Mental-Health.pdf
- Georgia Bowker-Brady, Advanced Specialist SLT (Berkshire Healthcare Foundation Trust) describes how using Talking Mats in dementia care and acute health patient inpatient services helps patients organise their thoughts and express what is going well for them, as well as what isn’t. https://www.talkingmats.com/acute-mental-health/
- Rachel Woolcomb, Talking Mats OT Associate, explains why Talking Mats supports thinking, and why it can be particularly useful in helping people to structure and express their thoughts. https://www.talkingmats.com/talking-mats-as-a-thinking-tool/
We would love someone to carry out some research in this field, so if this sparks a research, or blog idea, please get in touch with us at info@talkingmats.com.
Many thanks to Edith Barrowcliffe from The Action Group for sharing her experiences of using Talking Mats to support counselling with adults who have cognitive or communication difficulties. Watch this space for Edith’s follow-up blog next week which will describe how she has continued to use Talking Mats during lockdown. Please note that the image used in this blog is from a mock session and has been taken for publicity purposes only.
Eleven years ago, I began working at The Action Group with adults who have additional support needs and was struck by how many had mental health difficulties that they were getting little help with. Sadly, with services scarce enough for the “mainstream” population, I could see why.
The issue resurfaced for me in 2016 when I began training as a counsellor. I kept returning to whether talking therapy was possible with those who had difficulty communicating – or even thinking about – their feelings.
Then in 2019, I attended Talking Mats training. Immediately excited by the potential for emotional connection, I signed up for the advanced “Keeping Safe” training and approached The Action Group’s CEO with the beginnings of a plan.
I’m fortunate in working for an organisation willing to take new ideas and run with them. Within six months I was embarking on a pilot project, called HearMe, offering counselling to adults with cognitive or communication difficulties, with Talking Mats as a key method to help overcome those barriers. Within a fortnight of opening the service was full to its limited capacity and had a waiting list!
The work has been experimental, learning as I go and adapting to the particular needs of each client. To conduct initial assessments, I’ve assembled symbols based on “Thoughts and Feelings” from the “Keeping Safe” pack. We return to this to review progress. Most clients have used a top scale of “True”/ ”Not True” with statements “about me” for the assessment. We always begin with a practice mat based on more neutral material, allowing the client (Thinker) to learn what’s involved and me to gauge whether the mat is right for them. This is crucial – one client found a way to frame everything we placed on the mat positively even when they’d been able to tell me the opposite was true a moment before! In this case we simply used each symbol as a focus for exploration.
We’ve kept the number of questions relatively small, but the assessment can take two or three sessions to complete as clients often respond quite deeply to the symbols.
Some more verbally able clients move on to a more “freeform” style of counselling as we progress, relying less on the mat to open up. But even in these cases having symbols on hand can be helpful. One client brought up the topic of sex – then apologised and asked if it was OK to talk about it.
“It’s fine,” I was able to reassure her, producing the relevant symbol. “Look, we even have a picture for it”. She laughed and visibly relaxed, the card giving her tangible evidence that the topic was allowed.
It’s still early days, but from the feedback we’ve received so far, the project really seems to be helping people to open up, express feelings they’ve never given space to before, and explore ways they want to change their lives. The power of simply being heard.
Edith Barrowcliffe, Hear Me, The Action Group
With thanks to our funders and partners for making this work possible – Hospital Saturday Fund, The Action Group Board, Leith Benevolent Society, Port o’Leith Housing Association, and The Scottish Government. And to the team at Talking Mats for their support and help!
Follow the link below to find out more about our Keeping Safe training (now available online) and resource:
https://www.talkingmats.com/keeping-safe-a-new-talking-mats-resource-available-to-purchase/
We are delighted that we now have around 20 members of our Talking Mats (TM) research group. Members come from a variety of countries including the United Kingdom, Denmark, Cyprus, Germany, Sweden, Australia and Japan! We are a mix of academics and practitioners, with many combining both roles. So far we have spent time getting to know one another via video sessions and thinking about how the group might work.
We have decided our initial focus will be thinking about ways of analysing the data that is generated from conversations that are supported by TMs. This idea was suggested by Nikita Hayden. Nikita is a PhD student at the University of Warwick exploring the outcomes of siblings of children and adults with learning (intellectual) and developmental disabilities. Part of her research has used TMs with children with severe learning disabilities and their siblings to further understand their sibling relationships.
The types of data generated have been rich, vast and varied, leading to an overhaul of Nikita’s initial plan to analyse her TM data. This has raised questions about how TMs are interpreted and analysed in a research context, and what scope there is for our group to explore and synthesise the analysis potential of TMs. This is a question that the TM team is often asked and so having some information on the different options would be useful.
TM discussions generate various types of data, including:
- The photograph of the mat (which symbols are placed under the various columns);
- The conversation generated during the discussion;
- The body language and facial expression of the ‘thinker’;
- The speed of placement of symbols;
- The symbols that are moved following feedback etc.
We would like to review existing publications that have used TMs as research data and think about possible methods of analysis. This may include consideration of both within and between group research analysis techniques. It may also involve exploring the potential of both traditionally qualitative and quantitative analysis techniques, such as thematic or conversation analysis, or by drawing on data from the symbol placements to provide pre-post evaluation data.
We hope to generate a list of guidelines about what you might need to take into account when considering how to analyse these data. A challenge when analysing TMs data, is how to handle the variation in the types of data collected between participants. For example, some participants may place a large number of symbols, whereas other participants may have placed relatively few. This raises questions about how we deal with ‘missing data’. In small samples, how can we conduct a pre-post evaluation where some symbols are missing for some participants? If some participants use a five-point scale, and some use a two-point scale, what numerical analysis potential is there, if any? How can we appropriately derive qualitative themes from across our sample if some of our participants were minimally verbal? What sorts of non-verbal cues have been analysed in research using TMs?
Please do share any ideas or questions you have with Jill Bradshaw, our Talking Mats Research Associate – J.Bradshaw@kent.ac.uk
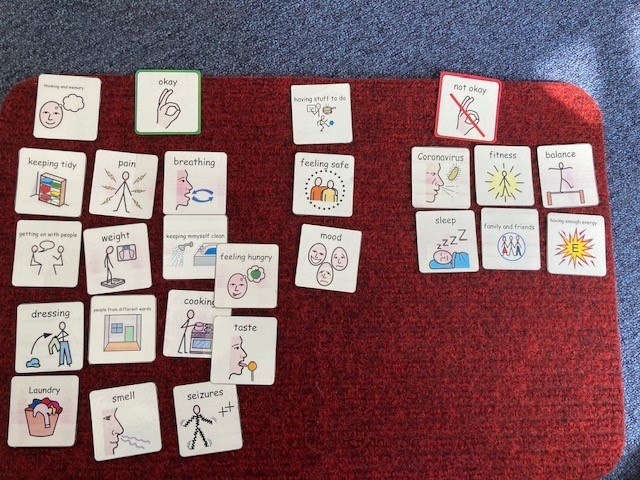
As a group of Allied Health Professionals (AHPs) working in a secure hospital we recently embarked on a mini project using Talking Mats to check in with our service users with learning disabilities during Covid-19. We collated the evidence from our respective professional bodies (Royal College of Occupational Therapy, Royal College of Speech and Language Therapy, Chartered Society of Physiotherapists and British Dietetic Association) in terms of changes that people might experience if they’d had Covid-19 and produced a talking mat around these.
It quickly dawned on us that we might be on to something here, and that creating an opportunity to ‘check in’ more broadly with our service users would serve a useful purpose, so we added some additional categories around changes to routine, psychological wellbeing and feeling safe.
This was my colleagues’ first experience of using talking mats, and their faces when I turned up clutching my 99p actual doormat were a picture! I introduced them to the theory behind the mat and its presentation and harped on about the benefits in terms of attention, comprehension, non-threatening interaction, initiation and structuring narrative; they nodded supportively.
We set off across our learning disability wards in multi-disciplinary pairs and all but a few of the service users agreed to have a chat with us. My colleagues commented that they were pleasantly surprised by the engagement and the amount and novelty of the information gained; we identified things that the service users hadn’t told anyone because they hadn’t been asked that question!
In talking to others we were asked why weren’t rolling this out in a partner secure hospital for people with mental health conditions? ‘no reason really, we just haven’t got there yet’ we answered. Then came the…. but we can just do it like a questionnaire with them. This question wasn’t, and in my experience isn’t ever ill meant. It comes from a place of naivety in relation to the presence of communication difficulties in people with mental health conditions and because of that, lack of exposure to different professional groups such as Speech and Language Therapy and the skills and approaches we have to offer. Skills in gaining and holding someone’s attention. Skills in decreasing pressure in communication situations. Skills in enabling time, space and ways in which people can initiate their thoughts.
The Multi-Disciplinary Team (MDT) working around the project has enabled me to show others how talking mats can support their practice. It has enabled them to see how a very simple and non-threatening visual tool can open up conversations and lead to information that the service users hadn’t shared before, in a way that a face to face conversation doesn’t.
Thanks to Jo Brackley, Clinical Lead, Speech and Language Therapy Secure Services at Cumbria, Northumberland Tyne and Wear NHS Foundation Trust for this inspiring blog – which demonstrates when we shift the way we listen and gather information from patients we get a different result and improve the quality of information and communication . If you or your team want to consider Talking Mats training then we can provide this for organisations . At the moment we can take a cohort through our online course together and then arrange a zoom call to discuss application to your work setting – email info@talkingmats.com for more information.
Our first Talking Mats advanced online module has launched. We are pleased we had developed our online foundation training well before lockdown. There has been such great feedback from people who have completed our online foundation course and they have been asking for more. They like the bite size chunks, being able to pace their own learning and the reflective practice approach. Now we are adding to our online course with an advanced Talking Mats module focusing on Talking Mats use in safeguarding. This course is structured around the Talking Mats Keeping Safe resource and how to use it.
The Keeping Safe Talking Mats resource was developed to check in with people and find out how their lives are going. It uses a holistic framework to do this and the conversation it supports is structured around three topics: 1) well-being; 2) relationships; 3) thoughts and feelings. The resource was trialled and tested in projects involving over 700 practitioners. Originally, it was designed for people with learning disabilities but feedback has been that it has been helpful with a wide range of people including, those with stroke, head injury, dementia and mental health issues.
The advanced online module involves 2 to 3 hours of learning that you do at your own time and pace. It involves short talks, reading, videos and reflective practice activities. You will develop confidence in using the resource as well as an understanding of relevant issues, such as diagnostic overshadowing, developing the capacity of individuals to raise concerns, the impact of trauma. You will be encouraged to reflect on how you can apply the Talking Mats Keeping Safe resource to your own area of practice
To apply for the course, you must have completed your foundation Talking Mats training. If you haven’t completed this training book now – there is still the reduced price training offer if you book your place before the end of August 2020. Access to this advanced course will begin on the first of every month and you will have the full month to complete it.
Book your place now. The cost is £85 for the course and the Keeping Safe resource and £35 if you already have your Keeping Safe resource and just want to do the training.
 Online training login
Online training login