Using Talking Mats to Explore How Children and Young People with an Intellectual Disability Feel About Undergoing Clinical Procedures
Many thanks to Greg Cigan for this great blog about his study that explored how children and young people with an intellectual disability feel about undergoing clinical procedures.
A clinical procedure is any activity performed by a healthcare practitioner to diagnose, monitor and/or treat an illness such as blood pressure testing, x-rays and other scans (Cigan et al., 2016). While some procedures cause no pain or only mild discomfort when completed, others can be prolonged and potentially painful (Coyne and Scott, 2014). Children and young people with an intellectual disability are more likely to develop physical illnesses including epilepsy and digestive disorders than the general population and can be frequently required to undergo healthcare procedures (Emerson et al., 2011; Short and Calder, 2013). Yet, there is currently little empirical research reporting how children and young people with an intellectual disability experience procedures (Peninsula Cerebra Research Unit, 2016). More research is required so that healthcare services can better understand the needs of children and young people with an intellectual disability (Oulton et al., 2016). As part of my doctoral studies at Edge Hill University, I am conducting a study that explores how children and young people with an intellectual disability experience having a clinical procedure.
From the outset of the study, I felt it was important to obtain data directly from children and young people rather than relying on parents and carers to speak on their behalf. I was keen to adopt methods during interviews that would enable as many children and young people as possible to take part, including those who find verbal communication challenging. After researching different methods, I chose to utilise Talking Mats as the innovative design of the tool offered children and young people the option to express their views entirely non-verbally should they wish to by arranging symbol cards. To date, I have interviewed 11 children and young people about their experiences of undergoing procedures. Each participant was between 7-15 years of age at the time of the interview and had a mild to moderate intellectual disability.
Prior to an interview beginning, I spent time describing and showing each child/young person a Talking Mat and asked whether they would like to use the tool during their interview. Out of the 11 children and young people I have interviewed, three used a Talking Mat. Those that chose not to use the tool were older children who were confident having a verbal conversation with me or those who had a visual disability and could not see the symbols. In all cases, the decision of the child/young person in relation to using the Talking Mats was respected.
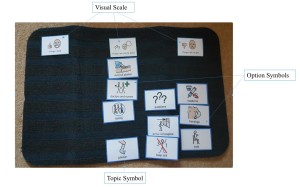
The three children who used the Talking Mats were able to express their views non-verbally and also seemed to convey more information than some of those who chose not to use the tool. Viewing the symbol cards within a Talking Mat appeared to help children and young people break down information into smaller chunks which then made it easier for them to process and discuss. Indeed, using a Talking Mat led all three children to discuss information that was new to their parents who sat in while s/he was being interviewed. An example of a completed Talking Mat is shown below which was created by an 11-year-old boy during his interview. The boy clearly expressed that he did not enjoy his experience of having a clinical procedure.
Within my study, I feel using Talking Mats has helped to augment the verbal communication of some of the children and young people which in turn enabled them to take part in interviews and share their views and experiences of procedures. Talking Mats are a valuable tool for researchers working within the field of intellectual disabilities. If used more widely, Talking Mats has the potential to enable more children and young people with intellectual disabilities to have the opportunity to be involved and express their views within healthcare research.
Reference List
CIGAN, G., BRAY, L., JACK, B. A. and KAEHNE, A., 2016. “It Was Kind of Scary”: The Experiences of Children and Young People with an Intellectual Disability of Undergoing Clinical Procedures in Healthcare Settings. Poster Presented at the 16th Seattle Club Conference (Awarded Best Poster Prize), 12-13 December. Glasgow: Glasgow Caledonian University.
COYNE, I. and SCOTT, P., 2014. Alternatives to Restraining Children for Clinical Procedures. Nursing Children and Young People, 26(2), pp. 22-27.
EMERSON, E., BAINES, S., ALLERTON, L. and WELCH, V., 2011. Health Inequalities and People with Learning Disabilities in the UK: 2011. Lancaster: Improving Health and Lives: Learning Disabilities Observatory.
PENINSULA CEREBRA RESEARCH UNIT, 2016. What’s the Evidence? Reducing Distress & Improving Cooperation with Invasive Medical Procedures for Children with Neurodisability. Exeter: University of Exeter.
SHORT, J. A. and CALDER, A., 2013. Anaesthesia for Children with Special Needs, Including Autistic Spectrum Disorder. Continuing Education in Anaesthesia, Critical Care & Pain, 13(4), pp. 107-112.
If you would like more information about Greg’s work you can contact him at Cigang@edgehill.ac.uk
 Online training login
Online training login