Many thanks to Georgia Bowker-Brady, Advanced Specialist SLT (Berkshire Healthcare Foundation Trust) for this latest guest blog.
I attended the Talking Mats training in June and I work in both dementia care and acute mental health in-patient services.
I had initially imagined that I would primarily be using the Talking Mats to support the dementia patients.
However I’ve been surprised to find that I have been increasingly using Talking Mats with functional patients and it has been a really positive tool when discussing with patients about their self-care, the care they are receiving in the hospital and opinions on discharge.
Due to their mental state, many of the patients may find it hard to organise and express their thoughts, and if patients are hypomanic it can be difficult for professionals to guide the topic to get meaningful information, but Talking Mats has really helped with this! It has also been pertinent in establishing patients’ insight levels and gaining better understanding of their impression of the current situation.
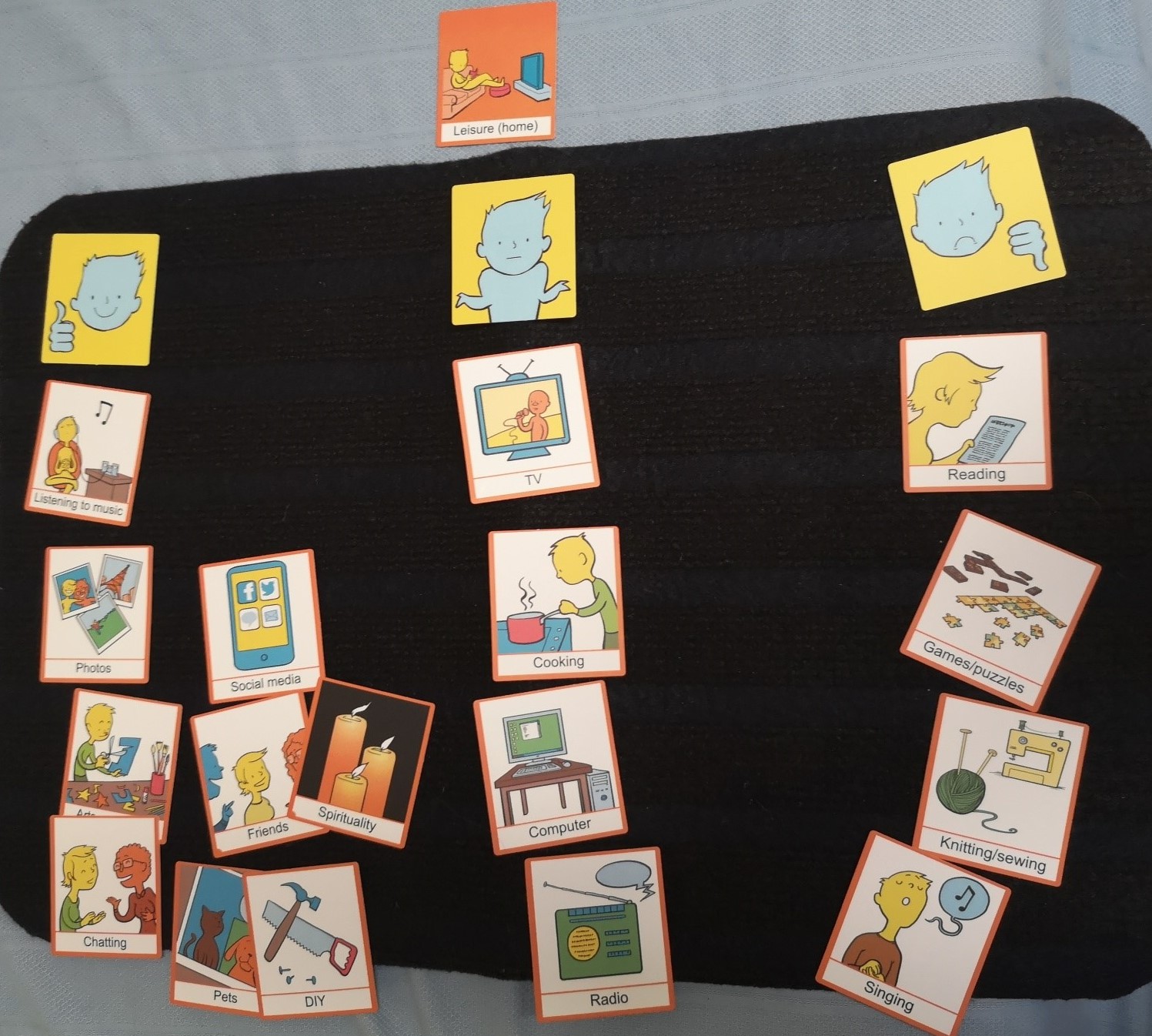
Here is a photo of one my mats from the psychiatric adult acute wards. This was for a patient who is severely low in mood and has relatively recently gone through a traumatic incident. The ward staff and OTs have had difficulty gathering any information about what she ordinarily enjoys doing in order find some activities to try and engage her with.
The staff stated that the patient would simply report she doesn’t enjoy anything and questions about what she used to enjoy received no answer. I went and did a joint session with the OT where I asked about what she enjoyed doing before this incident and we did the mat (see picture below) in a matter of minutes.
This can now provide a starting point for considering areas for trying to encourage some behavioural activation.
We then extended it by using an emotions wheel to ask how she felt about certain activities available in the hospital. We were able to establish that she felt fearful about trying new things and sad about carrying out certain activities she used to do prior to the incident.
It is wonderful to hear such a great example of Talking Mats in action – if you have any stories you would like to share, please get in touch with us at info@talkingmats.com
Many thanks to Claire Wiseman & Ann Lafferty from The Advocacy Project (Scotland) for this guest blog, including a great example of how Talking Mats helped a young woman with learning disabilities and psychosis share her views about being in hospital, receiving medical treatment and her preferences in respect of future post discharge welfare decisions:
For some time, The Advocacy Project have been thinking about how we could use the Talking Mats Framework to support people going through legislative processes such as the Mental Health (Care and Treatment) (Scotland) Act 2000, Adults with Incapacity (Scotland) Act 2000 and the Adult Support and Protection (Scotland) Act 2007.
Recently the Mental Welfare Commission published a best practice guidance on Supported Decision Making – https://www.mwcscot.org.uk/good-practice/guidance-advice, which we referred to as part of our presentation for the recent Talking Mats is 21 celebrations (click here to see the presentation Talking Mats and Supported Decision Making PP 2 (1)). The feedback from this session was that ‘yes’ there is a need for symbols to support legislation. As accredited trainers, we’ve also been asked when we’re delivering training to lawyers, Mental Health Officers, Social Workers, support workers and other advocacy organisations if there are specific symbols related to Supported Decision Making, particularly with regard to legislative issues.
Here is one of the Supported Decision Making and Talking Mats examples shared in our presentation:
One of our staff supported a young woman with a learning disability who was thought to be experiencing a psychotic episode. She had been detained in an in-patient learning disability unit under the Mental Health (Care and Treatment) (Scotland) Act 2003 on a Short Term Detention Certificate. The clinical team then made an application for a Compulsory Treatment Order, which was granted. Later, when discharge planning was in progress, an application for Welfare Guardianship was made under the Adults with Incapacity (Scotland) Act 2000.
Although the young woman was able to communicate verbally, the effects of the psychosis combined with her learning disability meant that her conversation was discursive and she was very easily distracted. Using a combination of Talking Mats and our additional symbols over a number of sessions, the advocacy worker managed to ascertain her views about being in hospital, receiving medical treatment and her preferences in respect of future post discharge welfare decisions.
The Talking Mats reports were submitted as evidence at two mental health tribunal hearings and the Welfare Guardianship hearing at the sheriff court. We received positive feedback from the Curator Ad Litem, Mental Health Officer and Sherriff regarding the reports as they had never had Talking Mats reports submitted before during these proceedings.
The use of Talking Mats had been instrumental in supporting the young woman to put forward her views and ensuring an outcome she was happy with.
Going forward, Talking Mats and The Advocacy Project will be exploring the possibility of a symbols set for Supported Decision Making and legislation. We are currently looking at funding possibilities.
A fantastic example of the power of Talking Mats – if you have any Talking Mats stories you would like to share, please get in touch! Just send me an email at laura@talkingmats.com
 Online training login
Online training login