Talking Mats is fun! Whether you are sitting on the floor completing your mat or sitting at a small table, young children enjoy the fact that they can give information through multiple channels – Talking Mats is visual, auditory and tactile. It is an engaging tool to use when consulting children.They can express a view without words if they want to or they can have a conversation if they enjoy chatting. Watching a young child thinking and reflecting about where they place their symbol on the mat can be a humbling experience. Some adults still consider young children as incapable of expressing their views or opinions but in reality they can often express strong views about things and are very capable of grading their responses. Sometimes we just don’t take the time to ask them about the issues in their lives and free up some time to listen.
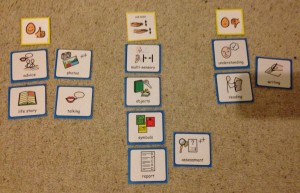
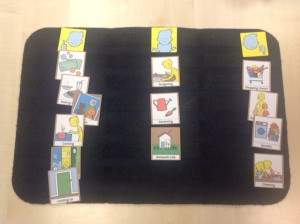
Talking Mats has created a specific Early years resource to make consulting young children easier. The symbols have been graded according to their developmental stage. When using the picture symbols it is important to remember:
- Most of the symbols in the Early years pack are concrete and you can quickly identify the shared meaning for example – “drawing”
- Others are concrete but have a broader meaning. An example of this is when asking about “eyes”
We have found that it is best to allow the child to interpret the meaning at their level so it maybe they have sore eyes; they don’t like their glasses or they have brown eyes. Try not to be too prescriptive when presenting the option to the child; a symbol can act as a jump off point capturing what fits for the child at the time. Just allow the meaning to emerge.
• The abstract symbols do need a bit more explanation because they ask about more complex concepts such as safety. The Early years pack asks about safety in relation to the road, physical safety and safety around others.
Asking about daily routines will give insight into how nurtured and cared for they feel. Let the child lead the discussion as much as possible.
Using visual communication is a great way to have a conversation with children in the early years and a good tool to involve children in decision making. Listening to the child’s view is essential for the GIRFEC process in Scotland and for co-producing Education Health care plans in England and Wales. Talking Mats has created a unique resource which is based on the “International Classification of Functioning, Disability and Health – Children and Youth version” Talking Mats uses a framework which helps children to express themselves in a way they feel comfortable with. As adults we need to be able to facilitate the conversation.
We find that to realize the full potential of Talking Mats it is best to attend a Talking Mats course . The courses allow you to focus on your situation and how you can be creative and apply it in your own work,
We are frequently asked if Talking Mats can be used by someone who is blind and we usually say ‘not really as its essentially a visual tool’. However today I had to eat my words when I was interviewed by Ian Hamilton who is a BBC Scotland TV and radio reporter. Ian is totally blind and was accompanied by his guide dog – a very large but gentle German Shepherd called Renton. Here is a link about Ian and Renton
When Ian asked me to explain Talking Mats I guided his hand to the positioning of the 3 top scale symbols and then he immediately understood the layout of the top scale, the topic at the bottom of the mat, and where to place each option by touch. I simply explained each symbol, placed it in his hand and he did the rest. The topic was how Ian feels about Domestic Life and we had a lot of laughs about his dislike of shopping, laundry and cleaning. He explained that shopping was a nightmare for someone who is blind. He said that the dislike of laundry and cleaning showed that he was lazy – I think it’s pretty much what lots of people think!
However he was clear about a number of things that he feels very positive about, in particular his daily routine and his security, both of which are very important because of his blindness. Interestingly he said that his guide dog is clearly on the positive side of the mat, but not as a pet. A dog like Renton is not just a form of mobility, he’s also a fantastic companion.
Ian seemed to keep 1 step ahead of me and asked loads of great questions about Talking Mats as a thinking tool and its possibilities for other groups of people. He commented that, like inventions such as the typewriter and the phone, Talking mats is something originally intended for people with a disability, but which is now being used by people of all abilities to help them consider issues and then express their views.
Ian generously agreed to me writing this blog and using his photo.
The programme will be broadcast on BBC Radio Scotland : Business Scotland on 24th and 25th May
During a research project funded by the Joseph Rowntree Foundation in 2007, Joan Murphy and Cindy Gray developed the Dementia Communication Difficulties Scale (DCDS) to help identify the communication difficulties that a person with dementia might be having and therefore help carers and staff to understand these difficulties and therefore support the person with dementia. The scale comprises 13 statements that are based on existing definitions of the communication problems commonly experienced by people as dementia progresses (Kempler, 1995; Health Education Board for Scotland, 1996):
In early stage dementia, the person
- may have difficulty coming up with words
- may tend to digress and repeat themselves.
In moderate stage dementia, the person
- may find it hard to understand what is said to them, particularly when being given complex information
- may have difficulty maintaining a conversation topic without losing track
- may use semantically empty words (e.g. thing, stuff) in place of content words
- may be difficult to understand.
In late stage dementia, the person
- may make little sense
- may not be able to understand what is said to them, even when simple language is used
- may often repeat what other people have said to them
- may communicate mainly in non-verbal ways
The DCDS requires a third party who knows the person with dementia well (a paid carer or family member) to assess various aspects of their communication on a 5-option scale. People are asked to circle the option that most closely describes the person in question.
Each DCDS option is assigned a score: for example ‘Never’ = 0, ‘Sometimes’ = 1, ‘Often’ = 2, ‘Always’ or ‘Says too little for me to judge’ = 3. A person’s DCDS rating is obtained by totalling their scores for all 13 statements. DCDS ratings can therefore range from 0-39, with a higher rating indicating a greater degree of communication difficulty.
The following stages of dementia group definitions were produced:
• DCDS ratings between 0 and 10.5 = early stage
• DCDS ratings between 11 and 19.5 = moderate stage
• DCDS rating between 20 and 39= late stage.
The Dementia Communication Difficulties Scale is brief, straightforward and quick to complete, and may therefore provide a highly useful tool for the care staff, clinicians and practitioners involved in assessing the needs of people with dementia.
If you would like a copy of the scale please click here: Dementia Communication Difficulties Scale
References:
Kempler, D. (1995). Language Changes in Dementia of the Alzheimer Type. In R. Lubinski (Ed.), Dementia and Communication, San Diego: Singular Publishing Group.
Health Education Board for Scotland (1996). Coping with Dementia: A Handbook for Carers. HEBS.
Using Talking Mats with Tony, a 53 year old man with learning disability and dementia. A guest blog by Rebecca Leighton Specialist Speech and Language Therapist and Consultant for elenbi-uk
“When I change I will be different”
Tony was referred to me for Speech and Language Therapy around 6 months after being diagnosed with mixed dementia. Dementia was having many effects on him but a key impact was communication difficulties: one of these difficulties was dysarthria (for him, this meant slow, slurred, effortful speech and difficulty maintaining enough breath support to finish his sentences) and another word-finding problems (difficulty remembering and producing the words he wanted to say – like the “tip of your tongue” phenomenon we all get from time to time, but occurring in most of Tony’s sentences). These two communication difficulties combined made talking very tiring and frustrating for him.
When I first met Tony, one of my aims was to find out what he wanted to achieve with Speech and Language Therapy. We discussed this but it was tiring for Tony and it became clear very quickly that using words alone was not helpful. It also became clear in that first session that although Tony was concerned about his speech, he was more concerned about his future and other areas of his life. He was worried about how he would enjoy life with dementia. He knew he would get worse and he wanted to know how he and his family would cope with that. Tony said “When I change I will be different. What will I do with myself?”
I introduced Talking Mats to Tony at our next session, suggesting that it would be a way of exploring what he was worried about in terms of his overall health and wellbeing and also what he might want from Speech and Language Therapy. We did four Mats over the course of two sessions:
Mat 1: Starter topic (food). Tony managed a three-point scale easily (“like” “dislike” and “not sure”) and told me “This is alright, its easy. I can talk if I want. But I don’t have to.”
Mat 2: “My worries”. Tony used a three point scale to indicate whether he was “not worried”, “a bit worried” or “very worried” about a range of aspects of his life and future. We found that Tony’s main worry was what he would do with his time as his dementia progressed.
Mat 3: “Activities with dementia” – a sub-mat based on Tony’s main worry identified in Mat 2. This was done jointly with his advisor, Sabira, from his local dementia support service, who planned the mat with me to ensure it covered all the options Tony had available to him locally. The mat revealed that Tony was already attending a well-being café but wanted to try other well-being cafes too, to meet more people. He was keen to try the singing group and also felt that his family needed support. Sabira commented that she thought Talking Mats should be used more with people with dementia and she intended to explore this within her own service.
Mat 4: “What I want help with from Speech and Language Therapy”. Again we used a three point scale, this time to indicate “yes”, “no” and “maybe” to possible goals for Tony. Options included assessment, therapy and advice. We chatted around each topic, giving Tony more information on each possibility and discussing if and how it could benefit him. Tony made informed choices around each option, and made the decision to start by creating a Life Story.
With Talking Mats, Tony has been able to give his full views on some very difficult topics for him. He has done so in a way which has reduced the demand on his speech, which made the discussion easier and less tiring for him. He has taken control of his Speech and Language Therapy care and has made informed decisions about his therapy goals. Perhaps more importantly he has taken control of his future and made informed choices about what he wants for himself and his family for the rest of his life.
Talking Mats could be used by many services for people with dementia. Imagine how empowered people with dementia would be, for example, if their social worker or dementia adviser were able to use Talking Mats with them to identify their needs and wishes and help them choose what they want for their present and future. What better way to involve people in their own care?
The only caveat? Get in there early. Empower people to tell their story while they are still able to use pictures and words to do so. Dementia can steal these skills, burdening families with making decisions on behalf of their loved ones. As a daughter, mother, wife and sister myself, I know I would feel much more at ease with making a decision for my relative with prior knowledge of what they themselves would have wanted. Talking Mats is one way of finding that out.
In the Health and Well-being resource, we have provided four sets of symbols to help people consider how they feel about their communication. Because communication is complex and often abstract, it can be particularly difficult for people to express their views about it, especially if they have existing communication difficulties. To make this easier, we have divided communication into four topics:
- Expression
- Understanding
- Learning and thinking
- Relationships.
In the following example, I show how each topic can be used to build up a picture of how someone feels about different aspects of their communication. I worked with Kate, a 42 year old woman who had a stroke which left her with severe expressive and receptive aphasia. She was able to communicate through vocalisations and gestures. She could sometimes draw or write down words and needed to point to ‘yes/no’ in order to reliably answer closed questions. Following discharge from hospital, I used Talking Mats with Kate to find out how she felt about her communication. I started with the ‘communication – expression’ topic and found that she felt that she was having lots of difficulties making herself understood, particularly on the phone and in group situations:
I then explored how Kate felt about understanding what people were saying to her. Kate was able to tell me that she found it easier to understand people on a one to one basis rather than in a group setting. She indicated that it really helped her if people used gestures or wrote things down. Her main difficulty was understanding people on the phone, and in fact she had stopped answering the phone altogether (see mat below).
We went on to do a mat about Kate’s learning and thinking. In this set, there are symbols which cover higher level language activities such as reading, problem solving and organisation. When we talked about these areas, Kate was able to tell me about the things she was finding most problematic, but could also identify some things that she felt she could still manage (such as calculations and reading newspapers).
I then asked Kate how she felt about communicating with different people in her life. This mat shows that Kate found talking to her husband and her parents (who lived quite far away) particularly difficult.
As a result of doing these mats, we were able to target the things that mattered most to Kate in relation to her communication, and came up with the following actions:
1. Kate felt that her husband needed support and information, so we spent time working with him, showing him the best ways to support Kate’s communication.
2. Because Kate’s parents lived quite far away, she could only contact them using the phone, which was very difficult. We worked on getting Skype set up so that Kate could communicate with her family using all the modes available to her.
By splitting communication into different sub mats, Kate was able to think about different aspects of her communication and identify the things that she found most challenging. Together we began to work out some ways to help her overcome her difficulties.
Use the communication symbols to find out what people want to work on and use a collaborative approach to establish some goals to work on in therapy. I used the original Talking Mats when I explored Kate’s communication with her, but you could do the same with Digital Talking Mats. Find out more about it here.
Within the Health and Well-being resource there are four symbol sets (health, looking after yourself, communication and leisure & environment). Within the ‘health’ set, there are three topics which can be used to help people express their views about different aspects of their health:
• Health
• Coping
• Mobility
I worked with Pete who had severe aphasia. Pete had a range of health problems, including epilepsy and high blood pressure. Pete found it very difficult to communicate with his GP, and usually relied on his wife to translate. This meant that not all of Pete’s health problems were addressed or discussed when he went to the doctor, and he often felt excluded from conversations at these appointments. Prior to one of Pete’s GP appointments, I used Talking Mats with Pete to find out how he felt about his health. During our discussions, Pete was able to tell me that he was worried about a number of issues, but he especially wanted to talk to his GP about his ears, as he was having a lot of pain and also had a ringing sensation in his ears which meant that he found it very difficult to concentrate, particularly when watching TV.
Pete took the photo of his completed mat with him to his next GP appointment and his GP used this as a focus for discussions. As a result, Pete was referred to an audiologist for assessment. His GP also spent time discussing Pete’s epilepsy with him and referred him back to the epilepsy specialist nurse who worked with Pete and his wife to improve their understanding and management of it.
Using Talking Mats helped Pete prepare for his GP appointment and also ensured that his GP focused on what was important to him. As a result, time was spent more effectively by all and Pete felt listened to and really participated in his GP consultation.
Use the Talking Mats ‘health’ symbols from the health and well-being resource to help people prepare for appointments with health professionals and manage their health more effectively.
When people have been in hospital for a period of time, for whatever reason, consideration needs to be given to discharge planning. There are often concerns about what a person may manage to do independently when they get home, and this often has an impact on where people are discharged to and what type of support they might need.
The ‘looking after yourself’ symbol sets in the health and well-being resource provide a good starting point for exploring some of these issues. This set is made up of three topic sets:
- Domestic life
- Self-care
- Work/education
I used these when I worked with a woman (Ruby) who had severe receptive and expressive aphasia. She had been discharged from hospital with a care package (carers came in three times a day to help her with personal care, meal time preparation and housework). Ruby had difficulty communicating through speech but was able to use Talking Mats effectively to express her views. I used the ‘domestic life’ symbols to find out how Ruby felt about managing the daily running of the household. Ruby was able to tell me that she felt she could now do more things around the house, such as hoovering and the laundry. She was ‘unsure’ about cooking and shopping, but indicated that these were areas that she wanted to work on.
Using Talking Mats, Ruby was able to tell me that she wanted to try to do more things for herself. We used photographs of the completed mats to discuss these issues in more detail with Ruby’s social worker and her husband. Initially, Ruby’s husband was hesitant about her doing more things around the house, but seeing the mat in front of him meant that he really listened to her views and felt happier about her taking risks and trying things for herself. As a result of our discussions, Ruby’s social worker reviewed her care package. She reduced the daily visits by carers and Ruby was given support from the rehabilitation team to help her work on preparing meals. Her husband arranged for a friend to take her to the supermarket once a week so that she felt more in control of the cooking. Use of Talking Mats meant that Ruby was really involved in setting her rehabilitation goals and ensured that her views were heard when her care package was reviewed.
The ‘looking after yourself’ symbols can be used to include people with communication difficulties in the decision making process. This is particularly important given the current legislative drive to promote self-directed support. Find out more about how to use Talking Mats by signing up for a training course at Talking Mats.
 Online training login
Online training login