We are excited by the growing use and impact of Talking Mats in CAMHS. With this in mind, we have updated our compilation of mental health blogs, and are pleased to share a new compilation with you. If you have used Talking Mats in a mental health setting and would like to share your experiences with us, please do get in touch at info@talkingmats.com – we would love to hear from you!



You can also access the blogs listed above by clicking the following links:
We are delighted to share a poster from Licenced Trainers Brid Corrigan and Libby Mills of NHS Greater Glasgow & Clyde, and Student Speech and Language Therapist Heather Pollock, developed as part of an Impact Project with the University of Strathclyde.
The poster reports on an evaluation of the impact of Talking Mats training on clinical practice across several Child and Adolescent Mental Health Services (CAMHS) in and around Glasgow. We were thrilled to hear the poster had been accepted at the Solving the Mental Health Crisis: Global Solutions Across the Lifespan Conference, held on Friday 21st June.
The project demonstrates how Talking Mats can be used by several members of the multidisciplinary team to build rapport and set goals with young people in both the inpatient and community CAMHS setting. A huge well done to everyone involved in the project for shining a light on how Talking Mats can help to hear the young person’s voice as part of their CAMHS journey.


We are pleased to share a new blog from Talking Mat Associate, Jess Lane, as part of a 2-part series on the use of Talking Mats within Child and Adolescent Mental Health Services (CAMHS).
In Part 1, Jess described how Talking Mats can provide children with a safe space to explore topics that they might otherwise feel unable to communicate about, in a way that is highly supportive, sensitive and impactful. Check it out here:
In Part 2, Jess reflects on the use of Talking Mats by all members of the multidisciplinary team. We also hear from Nikki Low, Specialist Occupational Therapist, who reflects on her use of Talking Mats in the acute mental health setting.
Later in the blog, Jess explores how Talking Mats can be used as part of a post-diagnostic package of support for autistic children to support more focussed, strengths-based conversations, in line with the core principles of neurodiversity affirming practice.
A Multidisciplinary Approach
Welcome back to my 2-part series on the use of Talking Mats within CAMHS. In Part 1, I described how the implementation of Talking Mats by all members of the multidisciplinary team has transformed the way children are supported in the acute mental health setting. I have since reflected with clinicians from across Speech and Language Therapy, Nursing, Psychiatry, Dietetics, Occupational Therapy, Physiotherapy and Psychology on how Talking Mats continue to be used on CIPU to facilitate the direct and meaningful involvement of children in care planning, and to facilitate equity of access to therapeutic intervention.
Nikki Low reflects on using Talking Mats in her role as a Specialist Occupational Therapist:
“I am a Specialist Occupational Therapist working in a Psychiatric Inpatient Unit with children under 12, many of whom, in addition to their mental illness, have an intellectual disability, are neurodivergent and/or have experienced complex trauma. This can make meaningful interactions about thoughts and feelings challenging or even impossible, particularly when discussing sensitive topics.
We strive to provide a client centred approach to care and treatment for our young patients but this can be difficult when they are unable to express themselves. Talking Mats has revolutionised our approach with these children. It has proven to be a powerful tool, transforming communication experiences for individuals of all abilities. I have used Talking Mats to engage patients in assessments and to formulate their treatment goals. Its user-friendly design, customisable features and positive impact make it an invaluable resource in the care and treatment of our vulnerable young patients.
As a unit, we have rolled out training to all core staff in order that we can incorporate Talking Mats into our practice. By doing this, we have been able to facilitate more inclusive and person-centred interactions, ultimately fostering a more supportive and empowering environment for all involved.”
Implementing Talking Mats across a whole staff team has increased the capacity and capability of clinicians to routinely involve children in decisions pertaining to their care. It has also contributed to a culture whereby Talking Mats are considered at each stage of a child’s admission, to support assessments of capacity and mental state, medication reviews, engagement with advocacy services and participation in all multidisciplinary team meetings and case conferences.
Post-Diagnostic Support
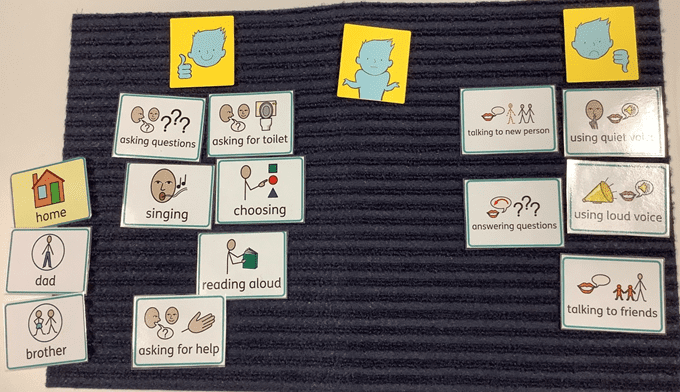
Most recently, I have used Talking Mats as part of a post-diagnostic package of support for autistic children, to support more focussed, strengths-based conversations around what it means to be autistic. This has involved developing a symbol set based on SIGN guidelines and associated resources, to support children who have recently been diagnosed as autistic, to engage in a conversation about what would be helpful for them to know.
When presented with a Top Scale of Helpful, Not Sure, Not Helpful, children were able to share their opinion on a range of options, including (but not limited to): facts and figures, autistic famous people, links to other work, skills, strategies and resources. An example is provided below. From this, I was able to create a personalised information pack for each child, based on what they would (and would not) find helpful to know about autism.

Most children shared that it would be helpful to find out about autistic famous people. This provided the foundation for a follow-up conversation about identity. Some children shared that they would find it helpful to find out about incidence and prevalence figures. Others did not. This was reflected in their information packs. For children who shared that they would like to understand how being autistic might impact, or otherwise feed into, therapeutic work for anxiety, I worked with colleagues from across Psychology and Nursing to ensure this was accurately reflected in their information packs.
Using a Talking Mat to scaffold conversations about what it means to be autistic has been well received by other clinicians involved in providing post-diagnostic support. By providing children with an opportunity to identify exactly what they would like to know about autism, clinicians have been able prioritise areas of support and signpost to the most relevant resources. This speaks to legislation that calls for the greater involvement of patients in decision making, in line with the mantra: no decision about me, without me.
Anecdotally, I have found that using Talking Mats as part of a post-diagnostic package of support has made a significant contribution to the development of a more streamlined, relevant and person-centred approach to sharing information. Using Talking Mats in this way has provided children with a dedicated space to voice their opinion on a topic that they might not have previously inputted into, that has been actively listened to and directly acted upon.
It is hoped that in sharing how Talking Mats can be used as part of a post-diagnostic package of support, this blog might encourage others to consider how they might achieve similarly positive outcomes for children with other diagnoses. If you have used Talking Mats as part of a post-diagnostic package of support for children or adults, I would love to hear from you! Please do get in touch at info@talkingmats.com.
Talking Mats is delighted to welcome a new Training Associate, Jess Lane. Jess has written this blog to introduce herself to the Talking Mats community. Welcome, Jess, we’re thrilled to have you as part of team TM!
Hello! My name is Jess and I am thrilled to be introducing myself as a newly appointed Training Associate for Talking Mats.
About Me
I am a Specialist Speech and Language Therapist with a clinical background in Learning Disabilities and Paediatric Mental Health. I also work for the Royal College of Speech and Language Therapists (RCSLT) as a Research and Outcomes Officer, where I help to build research capacity, capability and culture within the profession. I am currently studying towards a Clinical Doctorate in Professional Health Studies, looking at the use of Talking Mats for facilitating the direct and meaningful involvement of children in care planning.
Talking Mats has been a huge part of my career to date. This began in my hometown of Gloucester, where I worked as an SLT in an Intensive Support Service for children and adults with learning disabilities. Changes in my personal circumstances saw me relocate to Scotland in 2022, where I worked across Specialist Child and Adolescent Mental Health (CAMHS) Services in and around Glasgow. Most recently, I worked at a National Child Inpatient Psychiatric Unit (CIPU), supporting children with severe and enduring mental illnesses.
Talking Mats in CAMHS
Since completing my Licenced Training last year, I have been working with Talking Mats to deliver Foundation Training for CAMHS teams across the UK, as well as driving an upskilling initiative for Specialist Children’s Services locally in Glasgow. I have found that Talking Mats provides children with a safe space to explore topics that they might otherwise feel unable to communicate about, in a way that is highly supportive, sensitive and impactful. This is encompassed by feedback from a recent patient, who wanted to share that “using a Talking Mat is easier than talking because talking about how you feel can be difficult”.
Many of the children admitted to CIPU present with transient communication difficulties that can exacerbate the impact of mental ill health. Some children present with underlying communication difficulties that were not apparent in the community setting. Other children do not present with communication difficulties, but find it extremely difficult to think about, or share their views on, sensitive topics. Because of this, Talking Mats have been used extensively by the multidisciplinary team on CIPU to:
- Facilitate the direct involvement of patients in goal setting and care planning
- Adapt and extend traditional mental health inventions, including talking therapies
- Support capacity assessments, assessments of mental state and medication reviews
- Improve engagement with local advocacy services as part of the CTO process
- Adapt and extend assessments such as the Child Occupational Self-Assessment Tool
- Improve access to psychoeducation for patients with anxiety and/or depression
- Improve engagement with meal planning for patients with an eating disorder
- Support the differential diagnosis process for mental illnesses such as catatonia

Using Talking Mats in an acute mental health setting has transformed the way clinicians from across Nursing, Psychiatry, Dietetics, Occupational Therapy, Physiotherapy and Psychology engage with the children about their care and treatment. Feedback from the clinical team, children and their parents/carers has been overwhelmingly positive. Talking Mats are now used routinely on the unit to support children’s access to (and engagement with) therapeutic intervention as part of their wider recovery, as well as ahead of all multidisciplinary team meetings and case conferences to ensure each child’s voice is heard and acted upon.
I am so pleased to have joined the Talking Mats team and am very much looking forward to supporting other people to use Talking Mats in a range of settings. Stay tuned for a follow up blog on how I have used Talking Mats as part of a post-diagnostic package of support for autistic children and young people, designed to support more focussed, strengths-based conversations around what it means to be autistic, in line with the core principles of neurodiversity affirming practice.
This year’s campaign focuses on the importance of all children and young people whoever they are, and wherever they are in the world, to be able to say – and believe – “My Voice Matters.” Talking Mats is a tool that allows the voice of the young person to be heard. Read these blogs on Mental Health and Young People to find out more.
- Dr Carla Innes, Clinical Psychologist for Learning Disabilities at Stockport Healthy Young Minds (CAMHS) describes how Talking Mats helps the team to gain more insight to the children and young people they are working with, and how it has helped intervention focus on the child’s potential, and zone of proximal development.
- This work in Stockport is further expanded on in a presentation by Dr Rosie Noyce, Clinical Psychologist, given at the Talking Mats 21st Birthday Event in August 2019.
- Sally Kedge, SLT with Talking Trouble, New Zealand shares 2 powerful case examples of using Talking Mats with children and families caught up in the Criminal Justice System and demonstrates how the connection with a therapist can be the key to unlocking feelings and emotions
- Natalie Paris, Project Lead for Cashback180 programme based within Mayfield and Easthouses Youth 2000 Project, shares stories of using Talking Mats with young people in Midlothian.
- Our Director, Margo MacKay, describes using Talking Mats to ask young people about their environment and the impact different environments can have on wellbeing.
- Laura Holmes, our Lead Associate for Children and Young People, writes about the Virtual Schools Team in Wigan and how they used Talking Mats with Looked After Children.
To find out more about Talking Mats Foundation Training for you or your organisation, click here.
In the first of 2 blogs on Selective Mutism, Vanessa Lloyd of Birmingham Women’s and Children’s NHS FT describes using Talking Mats to give a young boy the opportunity to communicate at a time when talking was too hard.
Using Talking Mats with a primary school aged child with developmental Selective Mutism
Selective Mutism is a form of social anxiety characterised by stark differences in how a person communicates in different situations. There is also acute awareness of everyone around them who may be listening, either intentionally or accidentally. In Education settings Selective Mutism often become apparent at times of transition and teachers often describe a very different child to the one a parent knows at home. As a school therapist I have the job of finding the puzzle pieces and bringing them together in a way that home and school can understand. I have found the Talking Mats approach to be very useful when working in this area. Here’s an example;
I recently took a referral for ‘A’ who is 6 years old:
Main points from school:
- Joined 12months ago
- Not spoken at school in those 12 months
- Staff felt they didn’t know him
- Staff assumed he was happy not joining in
Main points from parents:
- Aware he is quiet in school
- This is who he is and he has been like this since starting Nursery
My observations indicated Selective Mutism;
- his body language indicated anxiety in situations where he was expected to speak or interact
I needed a way to feedback this anxiety to staff and for A to be heard without using his voice. After building a rapport with him I introduced Talking Mats and offered him the opportunity to engage
Getting Started
Using the Primary Communication Rating Scale (Johnson & Wintgens, 2016) as a basis, combined with an image system he was familiar with, I planned the symbols needed to support the conversation and set out the expectations for the activity. Fundamentally, I made it clear that he did not have to talk to me to participate.
How it went
The school environment.

As anticipated, he made his feelings instantly clear about the activities where he was required to talk, rapidly sorting them into ‘unsure’ or ‘don’t like’.
What was less expected was how relaxed his body language became, particularly when I suggested showing his class teacher. It was as though he knew that there was some power behind his arrangement of these symbols and he was ready to embrace it.
Follow up
Talking at home.
Having fully grasped the potential of the task, this young boy set to work answering my questions through careful consideration and placement of symbols. The same questions that would otherwise spiral him into a freeze or flee response were now being answered with a newfound command of the situation. He had things to say, things he wanted people to know, and in that moment, he had a way of doing this
Taking it forward:
Showing the child’s perspective provided a powerful way of highlighting to school the misguided assumptions that had been made about his feelings and attitudes towards talking. The Talking Mat conversations opened the discussion about the importance of Selective Mutism intervention and created a platform for the child to be involved and be heard. He was a valued contributor in an environment which was previously inaccessible for him.
This year’s campaign focuses on the importance of healthy connections in supporting mental health and wellbeing. Being able to communicate feelings and opinions is a huge contributor to creating healthy connections. Whether it is because there is a visual focus or because the ‘side by side conversation’ is more comfortable, Talking Mats is a tool that allows the voice of the young person to be heard. Read these blogs on Mental Health and Young People and our Impact Stories (to follow!) to find out more and take advantage of our discount on the Advanced Keeping Safe online module (details at bottom)
- Dr Carla Innes, Clinical Psychologist for Learning Disabilities at Stockport Healthy Young Minds (CAMHS) describes how Talking Mats helps the team to gain more insight to the children and young people they are working with, and how it has helped intervention focus on the child’s potential, and zone of proximal development. https://www.talkingmats.com/talking-mats-and-mental-health/. This work in Stockport is further expanded on in a presentation by Dr Rosie Noyce, Clinical Psychologist, given at the Talking Mats 21st Birthday Event in August 2019. https://www.talkingmats.com/wp-content/uploads/2019/08/Talking-Mats-and-Young-Peoples-Mental-Health.pdf
Sally Kedge, SLT with Talking Trouble, New Zealand shares 2 powerful case examples of using Talking Mats with children and families caught up in the Criminal Justice System and demonstrates how the connection with a therapist can be the key to unlocking feelings and emotions https: //www.talkingmats.com/support-for-prisoners-families-experience-from-new-zealand/
Natalie Paris, Project Lead for Cashback180 programme based within Mayfield and Easthouses Youth 2000 Project, shares stories of using Talking Mats with young people in Midlothian. https: //www.talkingmats.com/using-talking-mats-to-open-up-conversations-with-young-people/
- Our Director, Margo MacKay, describes using Talking Mats to ask young people about their environment and the impact different environments can have on wellbeing. https://www.talkingmats.com/consulting-children-impact-environment/
Laura Holmes, our Lead Associate for Children and Young People, writes about the Virtual Schools Team in Wigan and how they used Talking Mats with Looked After Children. https: //www.talkingmats.com/hearing-voices-looked-children-young-people/
Keeping safe is an Advanced Online Module and the first 20 people to sign up to this course will receive a 20% discount. Please remember you need to already be trained to Foundation Level to access this course. Use the code KS2020 at the checkout
We are all continuing to live in challenging times due to the COVID-19 pandemic, and there are concerns about the impact on the mental health of people at all ages and stages of life. This is a good time to reflect on the wide variety of blogs that have signposted how useful Talking Mats can be in helping people to think, structure coherent responses, and express their views. If this is an area of interest to you then take a look at these blogs to find out more:
- Debbie Mole, Clinical Nurse Consultant in Mental Health and Intellectual Disability for DHM Mental Health Care in Melbourne, Australia shares a great example of the positive impact Talking Mats can have for people who have experienced trauma. https://www.talkingmats.com/talking-mats-and-trauma-work/
- Natalie Paris, CashBack 180 Project Lead shares some powerful examples of how Talking Mats has helped her to open up conversations with the young people she works with https://www.talkingmats.com/opening-up-conversations-with-young-people/
- Edith Barrowcliffe from The Action Group demonstrates how Talking Mats has allowed individuals with intellectual disabilities access talking therapies and counselling. https://www.talkingmats.com/counselling-communication-1/
- Edith expands on this work in her second blog, describing how she adapted this approach to use during remote support during lockdown. https://www.talkingmats.com/counselling-learning-in-lockdown/
- Jo Brackley, NHS Clinical Lead for SLT Secure Services (Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust) describes how Talking Mats helps people with mental health open up and have richer conversations, with increased novel information gained. https://www.talkingmats.com/covid19_securehospitalsetting/
- Susan Gowland, SLT at NHS Fife Forensic Learning Disability Service, describes how Talking Mats support patients to express what they think in forensic learning disability setting. https://www.talkingmats.com/forensic_ld_setting/
- Dr Carla Innes, Clinical Psychologist for Learning Disabilities at Stockport Healthy Young Minds (CAMHS) describes how Talking Mats helps the team to gain more insight to the children and young people they are working with, and how it has helped intervention focus on the child’s potential, and zone of proximal development. https://www.talkingmats.com/talking-mats-and-mental-health/. This work in Stockport is further expanded on in a presentation by Dr Rosie Noyce, Clinical Psychologist, given at the Talking Mats 21st Birthday Event in August 2019. https://www.talkingmats.com/wp-content/uploads/2019/08/Talking-Mats-and-Young-Peoples-Mental-Health.pdf
- Georgia Bowker-Brady, Advanced Specialist SLT (Berkshire Healthcare Foundation Trust) describes how using Talking Mats in dementia care and acute health patient inpatient services helps patients organise their thoughts and express what is going well for them, as well as what isn’t. https://www.talkingmats.com/acute-mental-health/
- Rachel Woolcomb, Talking Mats OT Associate, explains why Talking Mats supports thinking, and why it can be particularly useful in helping people to structure and express their thoughts. https://www.talkingmats.com/talking-mats-as-a-thinking-tool/
We would love someone to carry out some research in this field, so if this sparks a research or blog idea, please get in touch with us at info@talkingmats.com.
In the UK we are emerging out of lockdown and there are concerns about the impact on the mental health of people at all ages and stages of life. This is a good time to reflect on the wide variety of blogs that have signposted how useful Talking Mats can be in helping people to think, structure coherent responses, and express their views. If this is an area of interest to you then take a look at these blogs to find out more:
- Edith Barrowcliffe from The Action Group demonstrates how Talking Mats has allowed individuals with intellectual disabilities access talking therapies and counselling. https://www.talkingmats.com/counselling-communication-1/
- Edith expands on this work in her second blog, describing how she adapted this approach to use during remote support during lockdown. https://www.talkingmats.com/counselling-learning-in-lockdown/
- Jo Brackley, NHS Clinical Lead for SLT Secure Services (Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust) describes how Talking Mats helps people with mental health open up and have richer conversations, with increased novel information gained. https://www.talkingmats.com/covid19_securehospitalsetting/
- Susan Gowland, SLT at NHS Fife Forensic Learning Disability Service, describes how Talking Mats support patients to express what they think in forensic learning disability setting. https://www.talkingmats.com/forensic_ld_setting/
- Dr Carla Innes, Clinical Psychologist for Learning Disabilities at Stockport Healthy Young Minds (CAMHS) describes how Talking Mats helps the team to gain more insight to the children and young people they are working with, and how it has helped intervention focus on the child’s potential, and zone of proximal development. https://www.talkingmats.com/talking-mats-and-mental-health/. This work in Stockport is further expanded on in a presentation by Dr Rosie Noyce, Clinical Psychologist, given at the Talking Mats 21st Birthday Event in August 2019. https://www.talkingmats.com/wp-content/uploads/2019/08/Talking-Mats-and-Young-Peoples-Mental-Health.pdf
- Georgia Bowker-Brady, Advanced Specialist SLT (Berkshire Healthcare Foundation Trust) describes how using Talking Mats in dementia care and acute health patient inpatient services helps patients organise their thoughts and express what is going well for them, as well as what isn’t. https://www.talkingmats.com/acute-mental-health/
- Rachel Woolcomb, Talking Mats OT Associate, explains why Talking Mats supports thinking, and why it can be particularly useful in helping people to structure and express their thoughts. https://www.talkingmats.com/talking-mats-as-a-thinking-tool/
We would love someone to carry out some research in this field, so if this sparks a research, or blog idea, please get in touch with us at info@talkingmats.com.
Many thanks to Edith Barrowcliffe from The Action Group for sharing her experiences of using Talking Mats to support counselling with adults who have cognitive or communication difficulties. Watch this space for Edith’s follow-up blog next week which will describe how she has continued to use Talking Mats during lockdown. Please note that the image used in this blog is from a mock session and has been taken for publicity purposes only.
Eleven years ago, I began working at The Action Group with adults who have additional support needs and was struck by how many had mental health difficulties that they were getting little help with. Sadly, with services scarce enough for the “mainstream” population, I could see why.
The issue resurfaced for me in 2016 when I began training as a counsellor. I kept returning to whether talking therapy was possible with those who had difficulty communicating – or even thinking about – their feelings.
Then in 2019, I attended Talking Mats training. Immediately excited by the potential for emotional connection, I signed up for the advanced “Keeping Safe” training and approached The Action Group’s CEO with the beginnings of a plan.
I’m fortunate in working for an organisation willing to take new ideas and run with them. Within six months I was embarking on a pilot project, called HearMe, offering counselling to adults with cognitive or communication difficulties, with Talking Mats as a key method to help overcome those barriers. Within a fortnight of opening the service was full to its limited capacity and had a waiting list!
The work has been experimental, learning as I go and adapting to the particular needs of each client. To conduct initial assessments, I’ve assembled symbols based on “Thoughts and Feelings” from the “Keeping Safe” pack. We return to this to review progress. Most clients have used a top scale of “True”/ ”Not True” with statements “about me” for the assessment. We always begin with a practice mat based on more neutral material, allowing the client (Thinker) to learn what’s involved and me to gauge whether the mat is right for them. This is crucial – one client found a way to frame everything we placed on the mat positively even when they’d been able to tell me the opposite was true a moment before! In this case we simply used each symbol as a focus for exploration.
We’ve kept the number of questions relatively small, but the assessment can take two or three sessions to complete as clients often respond quite deeply to the symbols.
Some more verbally able clients move on to a more “freeform” style of counselling as we progress, relying less on the mat to open up. But even in these cases having symbols on hand can be helpful. One client brought up the topic of sex – then apologised and asked if it was OK to talk about it.
“It’s fine,” I was able to reassure her, producing the relevant symbol. “Look, we even have a picture for it”. She laughed and visibly relaxed, the card giving her tangible evidence that the topic was allowed.
It’s still early days, but from the feedback we’ve received so far, the project really seems to be helping people to open up, express feelings they’ve never given space to before, and explore ways they want to change their lives. The power of simply being heard.
Edith Barrowcliffe, Hear Me, The Action Group
With thanks to our funders and partners for making this work possible – Hospital Saturday Fund, The Action Group Board, Leith Benevolent Society, Port o’Leith Housing Association, and The Scottish Government. And to the team at Talking Mats for their support and help!
Follow the link below to find out more about our Keeping Safe training (now available online) and resource:
https://www.talkingmats.com/keeping-safe-a-new-talking-mats-resource-available-to-purchase/
 Online training login
Online training login 



