The previous blog (read here) described the development of a set of symbols to prompt discussions around identity. In this blog, the authors illustrate how the symbols can be used to support practitioners to consider their own ideas about identity and how this may influence the clinical relationship.
The completed resource was trialled with practitioners working in a variety of settings.
Feedback
‘It help me understand and reflect on my own biases and how I am slowly working to be more aware of them and ask the right questions’
‘This Talking Mat was an eye opener about my worries and anxieties around saying the wrong thing’
Overall practitioners reported that using the resource helped;
• understanding and reflection on own biases and challenge default assumptions
• consideration of wider aspects of identity that were not routinely thought about
• holistic thinking by encouraging seeing clients in a wider context
• stimulate ideas about different questions to ask
• provide a safe platform for staff to open up
• address your own anxieties as a professional about getting it wrong and fear of ”putting your foot in it”.
It was also agreed that the resource could be used in diverse settings and not only within AAC.

Next steps
At the start of the process we were not sure where the discussions with the original project group would lead but the results of the pilot have shown that this Talking Mats identity resource is helpful for practitioners to mindfully reflect on their practice, allow unconscious bias to rise to the surface, consider all aspects of their clients’ identity to develop their practice, contribute to reducing inequalities and improving the responsiveness of services.
If you would like to know more about this resource and how it can support practitioners, please join Lois, Nikki and Lucia for an online webinar on
Tuesday 13th August 2pm – 3.30pm
Many thanks to Peter Just, Head of External Affairs, RCSLT and Padraigin O’Flynn, External Affairs Assistant, RCSLT for this blog describing the newly launched UK-wide RCSLT Survey, which includes free Talking Mats resources to support those with communication difficulties to have their voices heard.
Like many of you, the Royal College of Speech and Language Therapists (RCSLT) has been worried about the impact of COVID-19 on people with communication and swallowing needs. Based on what we’ve heard from our members, service user organisations and service users themselves we’ve been very concerned about how the UK-wide lockdown (March-June 2020) affected people’s access to the speech and language therapy they and their families and carers need.
To help us understand the issue better and to inform our response, we’ve just launched a UK-wide survey. Following consultation with service user organisations, the three key questions we’re asking are:
- How did lockdown affect your speech and language therapy?
- What impact did this have on you?
- What are your thoughts about the future?
From the start, we were clear: we wanted the survey to be as accessible as possible to as many people as possible, no matter how they communicate and no matter what their communication preference is. Over the past couple of months, we’ve worked with members to produce the survey in a range of accessible formats.
We’re particularly delighted that one of those formats is Talking Mats – and we’re very grateful to Lois and Laura for all their advice and support . As you will know better than anyone, the mats will enable people to give us their views and tell us how they’ve felt and are feeling. We are delighted the mats will provide people with the means to self-advocate – this will add a richness to the survey findings that they might otherwise lack.
We’ll be working with service user organisations to promote the survey to their networks. But we’d also really like your help too. Please share the survey and encourage as many people as possible to fill it out. The more voices we hear, the more stories we collect and the more responses we receive, the greater the impact of the survey findings will be.
Those findings, which we hope to publish early in the New Year, will be used to influence Governments, Parliaments and Assemblies across the United Kingdom. The case that will be making to ministers, officials and parliamentarians – that people must have access to the speech and language therapy they need – will be all the stronger for it being based on service users’ lived experiences. The very powerful testimony that the mats will provide will strengthen that case even further.
The survey is open until 5pm on Friday, 8th January 2021 and you can find more information about it here:
https://www.rcslt.org/learning/has-coronavirus-affected-your-access-to-speech-and-language-therapy
We hope you find the mats useful and if you had any queries or wanted any more information, please let us know. We look forward to working with you to help make a difference to the lives of people with communication and swallowing needs.
Peter Just, Head of External Affairs, RCSLT
Padraigin O’Flynn External Affairs Assistant, RCSLT
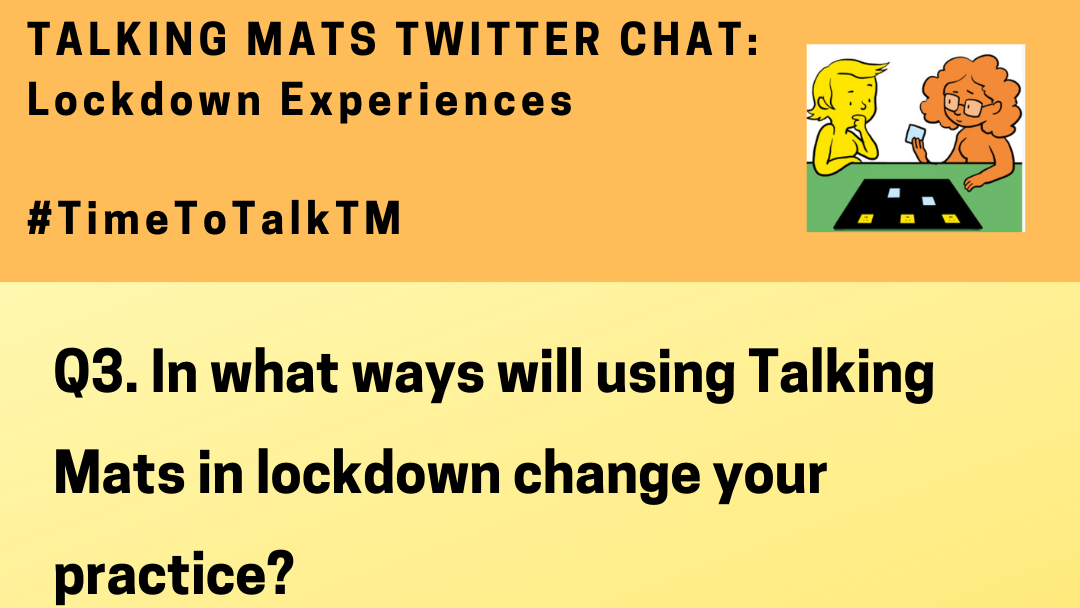
We are really looking forward to our first ever Talking Mats Twitter Chat on Thursday 01.10.20 from 7.30 – 8.30pm!
It will be a great opportunity to share experiences and ideas – here are the questions we will be asking:
This will be followed by a brief summary of the key learning points from the discussion. Join in and remember to use #TimeToTalkTM in all your comments – we look forward to chatting with you all!
We are delighted that we now have around 20 members of our Talking Mats (TM) research group. Members come from a variety of countries including the United Kingdom, Denmark, Cyprus, Germany, Sweden, Australia and Japan! We are a mix of academics and practitioners, with many combining both roles. So far we have spent time getting to know one another via video sessions and thinking about how the group might work.
We have decided our initial focus will be thinking about ways of analysing the data that is generated from conversations that are supported by TMs. This idea was suggested by Nikita Hayden. Nikita is a PhD student at the University of Warwick exploring the outcomes of siblings of children and adults with learning (intellectual) and developmental disabilities. Part of her research has used TMs with children with severe learning disabilities and their siblings to further understand their sibling relationships.
The types of data generated have been rich, vast and varied, leading to an overhaul of Nikita’s initial plan to analyse her TM data. This has raised questions about how TMs are interpreted and analysed in a research context, and what scope there is for our group to explore and synthesise the analysis potential of TMs. This is a question that the TM team is often asked and so having some information on the different options would be useful.
TM discussions generate various types of data, including:
- The photograph of the mat (which symbols are placed under the various columns);
- The conversation generated during the discussion;
- The body language and facial expression of the ‘thinker’;
- The speed of placement of symbols;
- The symbols that are moved following feedback etc.
We would like to review existing publications that have used TMs as research data and think about possible methods of analysis. This may include consideration of both within and between group research analysis techniques. It may also involve exploring the potential of both traditionally qualitative and quantitative analysis techniques, such as thematic or conversation analysis, or by drawing on data from the symbol placements to provide pre-post evaluation data.
We hope to generate a list of guidelines about what you might need to take into account when considering how to analyse these data. A challenge when analysing TMs data, is how to handle the variation in the types of data collected between participants. For example, some participants may place a large number of symbols, whereas other participants may have placed relatively few. This raises questions about how we deal with ‘missing data’. In small samples, how can we conduct a pre-post evaluation where some symbols are missing for some participants? If some participants use a five-point scale, and some use a two-point scale, what numerical analysis potential is there, if any? How can we appropriately derive qualitative themes from across our sample if some of our participants were minimally verbal? What sorts of non-verbal cues have been analysed in research using TMs?
Please do share any ideas or questions you have with Jill Bradshaw, our Talking Mats Research Associate – J.Bradshaw@kent.ac.uk
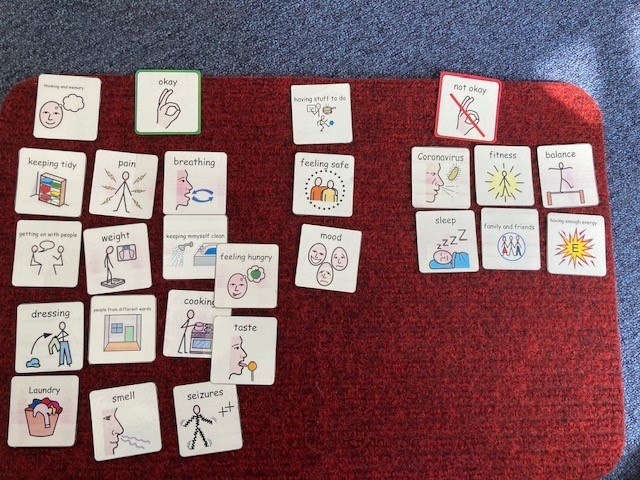
As a group of Allied Health Professionals (AHPs) working in a secure hospital we recently embarked on a mini project using Talking Mats to check in with our service users with learning disabilities during Covid-19. We collated the evidence from our respective professional bodies (Royal College of Occupational Therapy, Royal College of Speech and Language Therapy, Chartered Society of Physiotherapists and British Dietetic Association) in terms of changes that people might experience if they’d had Covid-19 and produced a talking mat around these.
It quickly dawned on us that we might be on to something here, and that creating an opportunity to ‘check in’ more broadly with our service users would serve a useful purpose, so we added some additional categories around changes to routine, psychological wellbeing and feeling safe.
This was my colleagues’ first experience of using talking mats, and their faces when I turned up clutching my 99p actual doormat were a picture! I introduced them to the theory behind the mat and its presentation and harped on about the benefits in terms of attention, comprehension, non-threatening interaction, initiation and structuring narrative; they nodded supportively.
We set off across our learning disability wards in multi-disciplinary pairs and all but a few of the service users agreed to have a chat with us. My colleagues commented that they were pleasantly surprised by the engagement and the amount and novelty of the information gained; we identified things that the service users hadn’t told anyone because they hadn’t been asked that question!
In talking to others we were asked why weren’t rolling this out in a partner secure hospital for people with mental health conditions? ‘no reason really, we just haven’t got there yet’ we answered. Then came the…. but we can just do it like a questionnaire with them. This question wasn’t, and in my experience isn’t ever ill meant. It comes from a place of naivety in relation to the presence of communication difficulties in people with mental health conditions and because of that, lack of exposure to different professional groups such as Speech and Language Therapy and the skills and approaches we have to offer. Skills in gaining and holding someone’s attention. Skills in decreasing pressure in communication situations. Skills in enabling time, space and ways in which people can initiate their thoughts.
The Multi-Disciplinary Team (MDT) working around the project has enabled me to show others how talking mats can support their practice. It has enabled them to see how a very simple and non-threatening visual tool can open up conversations and lead to information that the service users hadn’t shared before, in a way that a face to face conversation doesn’t.
Thanks to Jo Brackley, Clinical Lead, Speech and Language Therapy Secure Services at Cumbria, Northumberland Tyne and Wear NHS Foundation Trust for this inspiring blog – which demonstrates when we shift the way we listen and gather information from patients we get a different result and improve the quality of information and communication . If you or your team want to consider Talking Mats training then we can provide this for organisations . At the moment we can take a cohort through our online course together and then arrange a zoom call to discuss application to your work setting – email info@talkingmats.com for more information.
In our latest blog, Rachel Woolcomb, Talking Mats OT Associate, discusses how Talking Mats can support Reflective Practice for Occupational Therapists.
Taking time out to stop and reflect on our practice can be a challenge. We convince ourselves there are more important things to do, people to see, targets to meet, and therefore we just don’t have the time.
However, I suggest, that with this mind set we are doing ourselves, and the people to whom we provide support and care, a disservice.
Clinical supervision has always been embedded in the culture of occupational therapy and at its best should create a safe and supportive environment in which reflective practice can take place.
Unfortunately, in practice, the reality can look different.
The more I have used Talking Mats to enable my clients to think and express their opinions, the more I have been convinced, that there is also great benefit to them being used within the clinical supervision process.
I want to thank the occupational therapists who agreed to explore this further with me. They used Talking Mats to think about their coping skills at work, or reflected on how their ability to learn and think, impacted their job role.
They were surprised how easy they found it to think about the full breadth of their working life and the impact this had on their wellbeing. As clinicians, we are great at looking after other people and ensuring that their health and wellbeing needs are met, however, we are not so great at caring for ourselves.
The latest TMOT resource provides more information about why and how, Talking Mats can be an effective tool in enabling a reflective thinking space for clinicians. Check it out here: TMOT3 Reflective practice
Give it a go… You are worth it!
To find out more about our Talking Mats resources, check out this link:
https://www.talkingmats.com/shop/
 Online training login
Online training login