We are pleased to share a new blog from Talking Mat Associate, Jess Lane, as part of a 2-part series on the use of Talking Mats within Child and Adolescent Mental Health Services (CAMHS).
In Part 1, Jess described how Talking Mats can provide children with a safe space to explore topics that they might otherwise feel unable to communicate about, in a way that is highly supportive, sensitive and impactful. Check it out here:
In Part 2, Jess reflects on the use of Talking Mats by all members of the multidisciplinary team. We also hear from Nikki Low, Specialist Occupational Therapist, who reflects on her use of Talking Mats in the acute mental health setting.
Later in the blog, Jess explores how Talking Mats can be used as part of a post-diagnostic package of support for autistic children to support more focussed, strengths-based conversations, in line with the core principles of neurodiversity affirming practice.
A Multidisciplinary Approach
Welcome back to my 2-part series on the use of Talking Mats within CAMHS. In Part 1, I described how the implementation of Talking Mats by all members of the multidisciplinary team has transformed the way children are supported in the acute mental health setting. I have since reflected with clinicians from across Speech and Language Therapy, Nursing, Psychiatry, Dietetics, Occupational Therapy, Physiotherapy and Psychology on how Talking Mats continue to be used on CIPU to facilitate the direct and meaningful involvement of children in care planning, and to facilitate equity of access to therapeutic intervention.
Nikki Low reflects on using Talking Mats in her role as a Specialist Occupational Therapist:
“I am a Specialist Occupational Therapist working in a Psychiatric Inpatient Unit with children under 12, many of whom, in addition to their mental illness, have an intellectual disability, are neurodivergent and/or have experienced complex trauma. This can make meaningful interactions about thoughts and feelings challenging or even impossible, particularly when discussing sensitive topics.
We strive to provide a client centred approach to care and treatment for our young patients but this can be difficult when they are unable to express themselves. Talking Mats has revolutionised our approach with these children. It has proven to be a powerful tool, transforming communication experiences for individuals of all abilities. I have used Talking Mats to engage patients in assessments and to formulate their treatment goals. Its user-friendly design, customisable features and positive impact make it an invaluable resource in the care and treatment of our vulnerable young patients.
As a unit, we have rolled out training to all core staff in order that we can incorporate Talking Mats into our practice. By doing this, we have been able to facilitate more inclusive and person-centred interactions, ultimately fostering a more supportive and empowering environment for all involved.”
Implementing Talking Mats across a whole staff team has increased the capacity and capability of clinicians to routinely involve children in decisions pertaining to their care. It has also contributed to a culture whereby Talking Mats are considered at each stage of a child’s admission, to support assessments of capacity and mental state, medication reviews, engagement with advocacy services and participation in all multidisciplinary team meetings and case conferences.
Post-Diagnostic Support
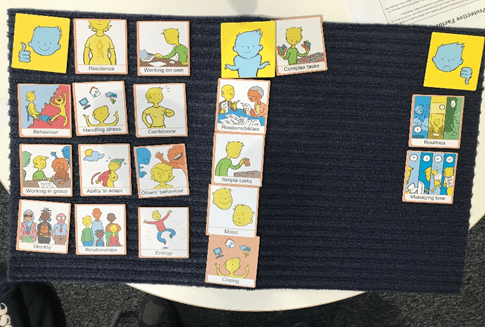
Most recently, I have used Talking Mats as part of a post-diagnostic package of support for autistic children, to support more focussed, strengths-based conversations around what it means to be autistic. This has involved developing a symbol set based on SIGN guidelines and associated resources, to support children who have recently been diagnosed as autistic, to engage in a conversation about what would be helpful for them to know.
When presented with a Top Scale of Helpful, Not Sure, Not Helpful, children were able to share their opinion on a range of options, including (but not limited to): facts and figures, autistic famous people, links to other work, skills, strategies and resources. An example is provided below. From this, I was able to create a personalised information pack for each child, based on what they would (and would not) find helpful to know about autism.

Most children shared that it would be helpful to find out about autistic famous people. This provided the foundation for a follow-up conversation about identity. Some children shared that they would find it helpful to find out about incidence and prevalence figures. Others did not. This was reflected in their information packs. For children who shared that they would like to understand how being autistic might impact, or otherwise feed into, therapeutic work for anxiety, I worked with colleagues from across Psychology and Nursing to ensure this was accurately reflected in their information packs.
Using a Talking Mat to scaffold conversations about what it means to be autistic has been well received by other clinicians involved in providing post-diagnostic support. By providing children with an opportunity to identify exactly what they would like to know about autism, clinicians have been able prioritise areas of support and signpost to the most relevant resources. This speaks to legislation that calls for the greater involvement of patients in decision making, in line with the mantra: no decision about me, without me.
Anecdotally, I have found that using Talking Mats as part of a post-diagnostic package of support has made a significant contribution to the development of a more streamlined, relevant and person-centred approach to sharing information. Using Talking Mats in this way has provided children with a dedicated space to voice their opinion on a topic that they might not have previously inputted into, that has been actively listened to and directly acted upon.
It is hoped that in sharing how Talking Mats can be used as part of a post-diagnostic package of support, this blog might encourage others to consider how they might achieve similarly positive outcomes for children with other diagnoses. If you have used Talking Mats as part of a post-diagnostic package of support for children or adults, I would love to hear from you! Please do get in touch at info@talkingmats.com.
Our thanks for this blog go to Deborah Little, Speech and Language Therapist; Clinical Lead for AAC & Total Communication (Children and Young People) NHS Dumfries and Galloway.
“Can we do a Talking Mat today Deborah? This is the question I am asked as soon as I enter the Learning Centre in one of our local schools by an enthusiastic 8 year old who has been exploring what completing a Talking Mat (TM) is all about this term. While we are in the early stage of this school’s TMs journey, the impact of embedding the approach into the fabric of how Children and Young People (CYP) are supported to communicate in school is already proving transformative.
Article 12 of The United Nations Convention on the Rights of the Child (UNCRC) guarantees children the right to express their views and opinions freely in all matters affecting them. The responsibility of ensuring children experience this right is also underlined in NICE guidelines (2022) that state: “Education, health and social care practitioners should always: put the life goals and ambitions and preferences of the disabled child or young person with severe complex needs at the centre of planning and decision making.”
Working with my teaching colleagues within one Additional Support Needs (ASN) setting this year, we reflected on how effectively the CYP were able to give their views and how consistently these views were acted upon in meaningful ways. We felt that this was an area we really wanted to improve upon and specifically we wanted to explore the following key questions in our minds:
- How can we support CYP’s understanding of their right to give their views and opinions? We reflected that for some CYP, their experience of being able to do this was very limited and that their understanding of using a TM was not yet at a stage where they were able to represent their views. We therefore wanted to prioritise finding out what helped these CYP to use TMs with understanding.
- How can we support CYP to know that they can tell us they aren’t happy about something? We reflected that during ‘Emotions Works’ discussion times many of the CYP routinely shared that they felt ‘happy.’ It was rare for the CYP to talk about unhappy feelings. We felt worried that the CYP often gave responses that they felt would be ‘right’ or pleasing to adults.
- How can we ensure we create a culture of prioritising time and space for CYP to share their views, opinions and ideas? We thought about opportunities throughout the school week that would create space and motivation for the CYP to engage with TMs. We wanted to achieve a feeling of TMs being integral to the everyday, as opposed to a sporadic ‘add on.’
To answer these questions, we agreed on the following key change ideas to implement and evaluate:
Developing understanding of the Talking Mats process linked with familiar learning opportunities.

Dynamic Assessment is an approach familiar to those working with CYP who use Augmentative and Alternative Communication (AAC). Adapting activities dynamically, being responsive to CYP’s progress, allows progressive skill enablement. Together with teaching colleagues, we applied this thinking to helping the children use TMs with understanding. If we had tried having a conversation using TM only a couple of times, our evaluation could have been that TMs wasn’t yet a tool we could use because for example, the CYP were putting all their symbols into the ‘I’m happy with this’ column only. Instead, we thought “OK, that’s where the CYP are now, let’s give them opportunities to practise engaging with this new tool and time to develop using the approach with understanding.” Put another way, we prioritised another key concept within the field of AAC: we Presumed Competence. We believed that the CYP had the ability to share their thoughts, feelings and ideas if we introduced TMs gradually, linking with the activities above, that were tangible and familiar to the thinkers.
Consciously modelling that is OK to have negative feelings and opinions.
When a CYP is learning what might be possible in terms of communicating with AAC, best practise is for supporting adults to model the AAC. This means, adults ‘use AAC to teach AAC.’ We show CYP that we highly value the AAC and want to use it too. We use it in real situations, modelling vocabulary to help CYP understand the symbolic vocabulary and how they can begin to use it too. When helping the CYP understand how TMs could help them express a wider range of emotions, we tried out using this approach. Now and again, supporting adults would share with the CYP how they were feeling about things using TMs and would include negative feelings.

One CYP had a memorable response to my sharing that I was feeling “not happy” with my cat. The CYP’s eyes widened and he became instantly animated, using his AAC to ask “cat..bad..what?” I was able to explain that my cat had been scratching my carpets and I was feeling upset about this. The CYP then used his AAC to say “cat…dig!” He pointed at the ‘not happy’ symbol in the Talking Mats top scale, jointly sharing his attention to this symbol and understanding of what this meant with me. The next week, we used TMs to ask this young person about a social group he had attended. For the first time, we noticed him ‘swithering’ across his top scale while making his choices. Also for the first time, I was confident that he shared his authentic feelings with me. I reflected on the power of modelling and normalising feelings that are ‘not happy.’
So, where are we now? The key themes from our findings after a year of using TMs as described above are:

In summary, using TMs in this setting has all supporting practitioners in agreement that it is not only important to listen to CYP when we know they might be having a tough time; we need to create space to listen all of the time, week to week, with authenticity and without agenda. The principles regularly used within AAC practice of: modelling, presuming competence and dynamic assessment have been effective in supporting more children to be able to experience their UNCRC Article 12 Right, more of the time and with increased understanding and confidence.
References
- UN Convention on the Rights of the Child – UNICEF UK
- NICE Guidelines [NG213] (2022) Disabled Children and Young People up to age 25 with severe complex needs: integrated service delivery and organisation across health, social care and education.
- Emotion Works www.emotionsworks.org.uk
- Daneshfar, S and Moharami, M (2018) Dynamic Assessment in Vygotsky’s Socioculturaly Theory: Origins and Main Concepts. Journal of Language Teaching and Research 9(3):600
- Donnellan, A (1984) The Criterion of the Least Dangerous Assumption. Behavioural Disorders, 9 (2), 141-150
- Sennott, Light and McNaughton (2016) AAC Modelling Intervention Research Review. Research and Practice for Persons with Severe Disabilties 41 (2)
Our thanks for this guest blog go to Meredith Smith, Paediatric Physiotherapist and Lecturer in Physiotherapy in the School of Allied Health Science and Practice at the University of Adelaide. In this blog, Meredith talks about the development of a Talking Mats resource to facilitate self-reporting in pain assessments for children and young people with cerebral palsy.
Our research team has been working on modifying pain assessment tools so they are more appropriate, relevant and accessible to children and young people with cerebral palsy (CP). People with CP have varying functional, communication and cognitive abilities, which makes existing assessment tools (often pen and paper questionnaires) difficult to use across the spectrum of ability. As a result, children and young people with CP often don’t have the opportunity to self-report how pain is impacting their function.
We are based in Australia and our team is made up of physiotherapists, an occupational therapist, a medical practitioner, researchers and people with lived experience of CP. One of the first things we did as part of this project was to ask people with lived experience of CP and clinicians what we could do to make two specific pain assessment tools more accessible and relevant to people with CP and different abilities. One of the clinicians (a speech pathologist), suggested we consider a Talking Mat alternative for each of the assessment tools. These two assessments focused on two concepts – 1) how pain interferes with function and 2) pain-related fear. We were keen to focus on these assessments as this would help us to not only open up a conversation about pain with children and young people with CP, but would also provide us with a way of identifying children who might benefit from particular pain interventions, and allow us to monitor the effectiveness of these interventions.
Prior to this suggestion I had heard of Talking Mats but never used it. Our research team underwent Talking Mats foundation training which was excellent, and we were all really impressed with the concept and its application in varying contexts. We had initially thought that we might need a Talking Mat to get feedback from children on the assessment tools, but we all agreed that converting the pain assessment itself into a Talking Mat would make the most sense for now.
Working with the Talking Mats team was a fantastic experience. We all really appreciated the expertise of the consultants in considering how we worded some of the assessment tool items. The symbols created were also excellent, and when we tested them with children and young people with CP they were simple and easy to understand.
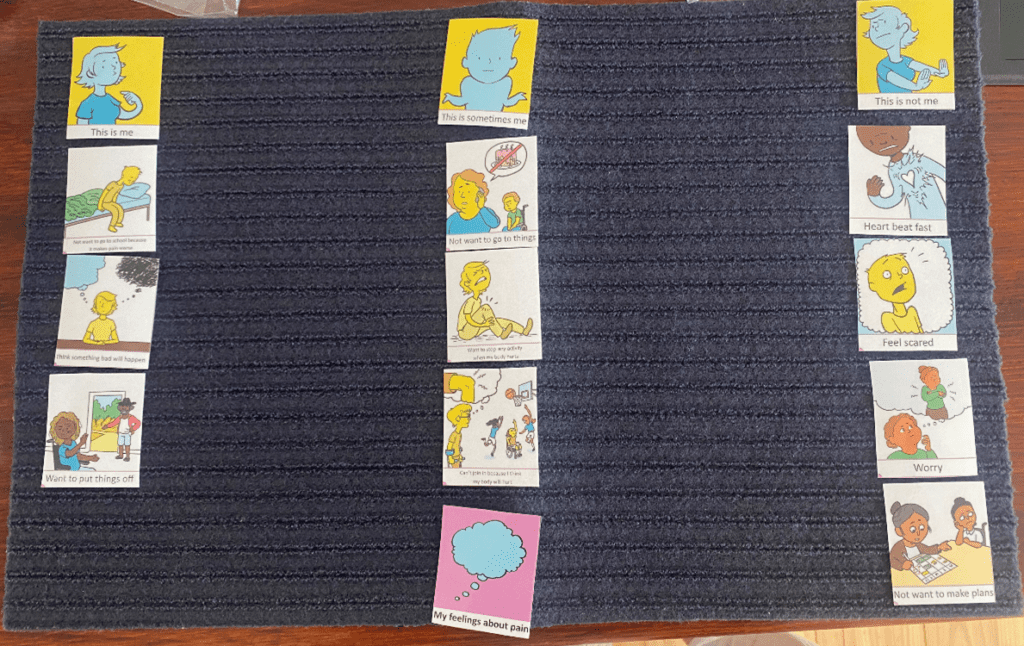
Here is an example of a Talking Mat discussing pain interference with function. The lead in phrase is ‘how much does pain get in the way of……’. This Talking Mat was easily understood by most children with CP, even those with moderate cognitive impairment and complex communication needs.

The second Talking Mat looked at pain related fear, with the lead in phrase ‘pain makes me……’. This was a more challenging and abstract concept, but was much easier to explore using the mat than on a standard pen and paper questionnaire. The Talking Mat versions can be interpreted as a 5-point response scale (the three response options and then two in-between sections), allowing us to still total an overall score for the assessment.
The feedback from children, young people and their families has been very positive. Families of children with cognitive impairment or complex communication needs have shared with us that previously it was assumed that their child could not self-report pain, and often they were asked to proxy-report on their behalf. Parents have told us how difficult it is to proxy-report on personal concepts such as pain-related fear, and that they couldn’t possibly know for certain how pain was making their child feel.
We are in the process of continuing to test the Talking Mats resource and look forward to making the it more widely available in the future.
Keep an eye on our website for more information about the Pain Assessment Resource as this project progresses.
If you are interested in completing Talking Mats Foundation Training, you can find out more here.
Talking Mats are delighted to share that we have been awarded funding to create a brand-new sensory resource for children and young people who have Speech, Language and Communication Needs (SLCN) and sensory integration/processing difficulties. The funding to create this resource has been awarded by the Communication Trust from the Communication Consortium Grants Programme – funded by The Rayners Special Educational Trust.
The Communication Trust Consortium, a coalition of over 35 not-for-profit organisations, is hosted by ICAN. They harness collective expertise to support the workforce and commissioners to support all children and young people’s speech, language, and communication skills across the UK.
This exciting year-long project will be led by Laura Holmes, our Lead Associate for Children and Young People. Laura has been part of the Talking Mats Team since 2016 and has over 20 years’ experience of working as a Speech and Language Therapist with children and young people, across a wide variety of settings in both NHS and independent sectors.

New Sensory Resource
This project will develop, pilot and launch a Talking Mats visual communication resource to tune into a child’s view of their sensory needs. It will enable children and young people who have speech, language, and communication needs (SLCN) and sensory difficulties to have a voice in their therapy assessment, planning and intervention.
“Sensory integration” and “sensory processing” refer to the processes in the brain that allow us to take the signals from our senses, make sense of those signals and respond appropriately. Children and young people with sensory processing/integration difficulties often have speech, language and communication difficulties, which may be linked to a diagnosis of autism (Green et al 2016); developmental language disorder (Simpson et al 2020); hearing impairment (Alkhamra et al 2020); or a history of trauma (Fraser et al 2017).
This work is important as sensory assessments can typically involve a mixture of formal and informal questionnaires and checklists which are carried out with Parents/Carers, Education Staff, and may also involve observations of the child in their environment. The issue is that Child Voice is not always routinely, or effectively, included in these assessments, or in subsequent planning and intervention – however the Royal College of Occupational Therapists recommends that ‘person-centred goals/outcomes must be established prior to intervention’ (RCOT, Informed View: Sensory Integration and Sensory-Based Assessments 2021). This also links with the current SEND system in England and GIRFEC in Scotland, both of which also emphasise the importance of child voice throughout assessment, planning and intervention processes.
We plan to work with experienced Talking Mats OT and SLT practitioners working with children and young people who have SLCN and sensory needs, to co-create this resource.
Get Involved
If you, or someone you know, works with children who have a diagnosis of SLCN and sensory needs, and is an experienced Talking Mats practitioner, please share the news about this project.
If this applies to the work that you do, and you would be interested in taking part in this project, please follow this link to express your interest: Communication Trust Project.
Expressions of Interest should be submitted by Friday 23/09/22.
Stay Connected
For more information about Talking Mats, please visit our website www.talkingmats.com or follow us on social media to keep up to date with all our news!
Many thanks to Natalie Paris, CashBack 180 Project Lead for our latest guest blog. Natalie shares some powerful examples of how Talking Mats has helped her to open up conversations with the young people she works with:
I joined Y2K Mayfield and Easthouses Youth 2000 Project in February 2018 as a sessional worker looking to gain practical experience in youth work, I then became Part Time Young Women’s worker at Y2K, which gave me experience in working with vulnerable young women in Midlothian across an age range of 11 to 24, some with mild to moderate learning difficulties. When I first heard about the 180 project, I knew it was something I really wanted to be involved with, as I have always been interested in Criminology and Youth Offending.
In September 2018 I became the full-time 180 Project Lead, and have helped to shape and develop our CashBack 180 Project. CashBack 180 is a referral-based service, focusing on early support and prevention for young people involved in or at risk of becoming involved in offending, anti-social and risky behaviours.
The Project:
We work with young people to make positive changes in order to work towards more positive futures. Young people accessing this service have the opportunity to take part in fun, participative and educational programmes of activities as well as 1:1 supports. The CashBack180 programme is delivered at Y2K, but we can also deliver programmes within High Schools.
CashBack 180 offers a menu of options and has adapted where necessary for our journey through the pandemic.
- 1:1 supports
- Groupwork programmes
- Community outreach support through detached youth work
Case Example 1:
A 12-year-old girl had been referred to me for violence, as she had attacked a girl in the playground, which was out of character for her. She was very uncomfortable in the 1 to 1 session, so I used a Talking Mat. This made the conversation flow more naturally.
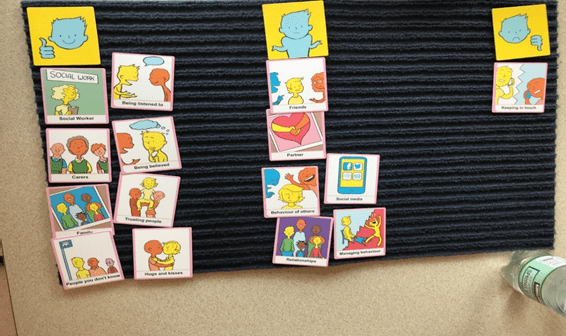
I used the Relationships topic, with the top scale ‘going well/okay/not going well’. This helped me get more information. I found out that most of the issues she was having were around peer relationships. For example, friends saying things that weren’t true, and not being believed by others in her friendship group. This allowed me to plan a session around what is healthy and unhealthy in friendships.

Case Example 2:
I was working with a 14-year-old care experienced boy, who had been referred to me for Anti-social behaviour, and because he was easily led. Once I got to know this boy a little better, I realised that he did not have much support within his family, apart from his older brother who he lives with now. I realised he was someone who had just learned to cope himself, and probably didn’t have many people to turn to when worried about things. I thought coping would be a good topic for a Talking Mat, as he always said things were fine, but I didn’t feel it was the full truth. I used the top scale ‘going well/okay/not going well’. This gave us the opportunity to discuss healthy and unhealthy coping mechanisms that he had and what he could do instead.
Case Example 3:
I was working with a 12-year-old care experienced boy, who had been referred to me due to his inappropriate sexualised language and reference to sexual experience. He has been out Mainstream school for 1 year, so had missed P7 sex education. I decided to start working on friendships and relationships over the first couple of weeks with him, to get an understanding of what he knew was acceptable in relationships. I used the Relationships Topic with the top scale ‘Going well/Okay/Not going well’. The Talking Mat helped me keep his attention for a little longer than usual, as he is a very chaotic young person and often gets up and walks about, or jumps on tables and pretends to be sleeping. It also showed me that he felt quite happy but was missing his friends from where he used to live. We are now looking at ways to address this.
Follow this link to Find out more about this project:
180 Service – Mayfield and Easthouses Youth 2000 Project
If you are feeling inspired and would like to know how you can access Talking Mats training, find out more here: https://www.talkingmats.com/training/
In the second of two blogs, we talk about how using Talking Mats Resources can help people have better conversations.
Our first Resources blog (https://www.talkingmats.com/resources-with-training/) focused on the resource bundles which are available to purchase with our Foundation Training course. This second blog focuses on the resources which are available to people who have completed our Foundation Training course.
Remember that most of our resources are available in both low-tech, and digital, formats.
Post-Training
Once you have accessed one of our Foundation Training courses, you can purchase our resources at a reduced rate:
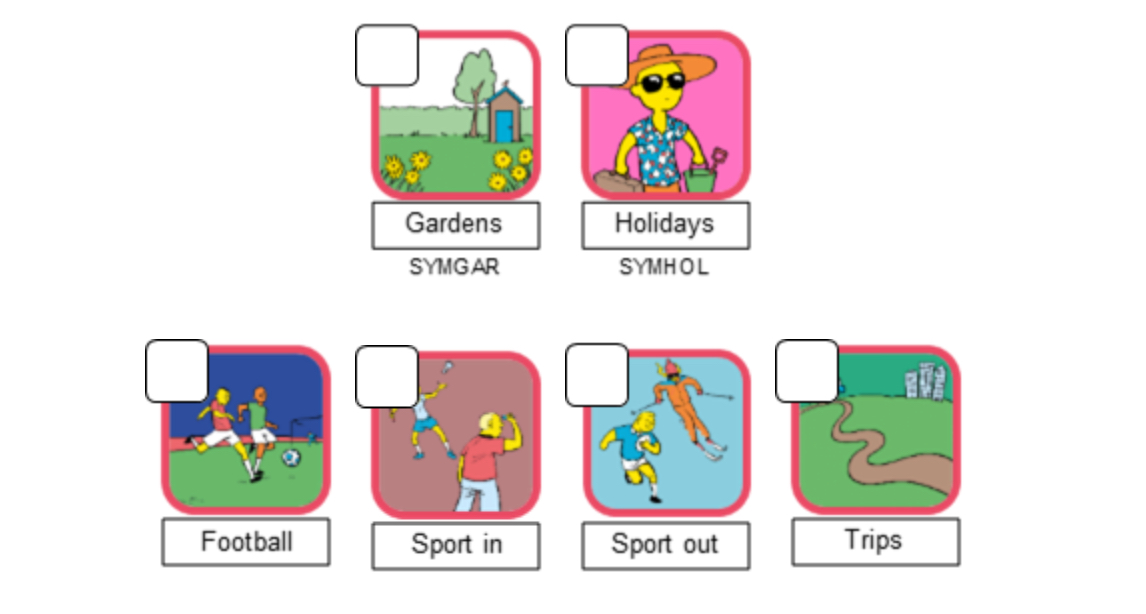
1. You can buy these in established sets using our post training order form, for example you may choose to buy a social care set, the secondary Children and Young people resource, or one of our Advanced sets (see 3. below). These sets all have 3 topics of conversation in them.
2. New for 2020! – you can now buy individual topics of conversation from our ‘pick and mix’ selection, which includes topics from our Health and Well-being Resource (also available as a bundle purchase with our Foundation Training course), as well as our Conversation Sets:
3. Our advanced sets, for example Keeping Safe and Thinking Ahead, are only available for those who have completed foundation training:
- Keeping Safe: Give people time to reflect on their lives and raise concerns using this resource. This can help you to explore sensitive issues in a non-threatening way by creating a listening space, simplifying abstract ideas, supporting thoughts while encouraging expression and decision making.
- Thinking Ahead: Support people to express their views and help them plan for end of life using this resource. It will also be helpful for many other people to consider future options in their lives.
We are also planning to add a ‘how was school today?‘ topic to our ‘pick and mix’ selection soon – so watch this space!
To find out how our resources could help you in your professional area of work/setting, check out these links here: https://www.talkingmats.com/where-you-work/
For more information about these resources please contact the office on 01786 479511 or email info@talkingmats.com
 Online training login
Online training login