This is the second of Kristine Pedersen’s projects using Talking Mats as a tool to support people with dementia.
Care workers at two residential care homes in Denmark were taught how to use the Talking Mats framework and how to incorporate the method into planning daily activities for people with dementia.
The care workers gave positive feedback in regard to using Talking Mats:
- Using the Talking Mat framework provides important knowledge about communicative difficulties of the person with dementia
- Talking Mats helps people to understand their options and thereby motivates to social activities, eating, physical exercise, etc.
- Talking Mats increases the possibility of active participation in caregiving plans
- Talking Mats enhances the joy of work, when I know how I can give the right care
- The Talking Mats conversations support a closer relation between elderly and care giver
This project and the one described in the previous blog, gave the opportunity to explore the Talking Mat framework in use and how the framework can support the communication of people with dementia. Very importantly, due to the adoption of Talking Mats and its extension in Denmark, the projects gave a lot of Danish examples. The projects also gave important information about how to implement the tool in care homes for people with dementia within a Danish setting.
‘We are very grateful to the Directors, Dr Joan Murphy and Lois Cameron and everyone on the team at the Talking Mats Centre who developed the framework and who continue to increase knowledge of Talking Mats through research and education. It is a very helpful tool for many people and supports and enables more people to have their views seen and heard’
And we are grateful to Kristine for sharing her projects with us.
We are very grateful to Kristine Pedersen from Kommunikationscentret in Denmark for sharing the findings of 2 projects with us. The first project found Talking Mats was effective in supporting communication for people who have dementia when compared with both unstructured and structured conversations.
‘t is important to know how to give people with dementia the right support’
At Kommunikationscentret in Hillerød (Denmark), we have been using the Talking Mats framework since our first trainer was accredited at the Talking Mats Centre, University of Stirling in 2010. We have been using Talking Mats with both children and adults across a range of communication difficulties e.g. caused by Aphasia, Cerebral Palsy, Downs Syndrome, learning difficulties etc. Inspired by the important research project by Dr. Joan Murphy and others ‘Decision making with people with dementia’ (2010), our next step was to gain our own experience within the framework specifically aimed towards people with dementia.
As in the rest of the world, the number of people in Denmark with dementia is increasing. Symptoms of dementia vary from person to person but many of the symptoms are related to communication: Difficulties finding words, using familiar words repeatedly, losing track in conversation, difficulties in focusing and paying attention etc. The growing dependence of the person with dementia on a caregiver makes communication essential to express wishes and needs. Therefore, it makes sense to look at the consequences of the illness (dementia) within the perspective of communication and how family members and professionals around the person with dementia can support communication using AAC.
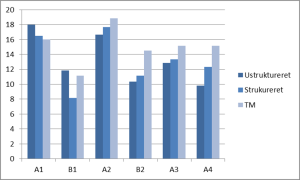
The purpose of the first project was to compare the communication in conversations about views on I) Daily activities and II) The importance of information, using three different communication methods. The methods were: 1) unstructured conversation 2) structured conversation 3) the Talking Mats framework. The project involved 6 participants having early to moderate stage dementia, all living in residential care homes.
Like the study ‘Decision making with people with dementia’ (2010), the report concludes that the Talking Mats method was associated with better communication for the majority of the participants. The Talking Mats framework was found especially helpful regarding the participant’s ability to understand subject and question of the conversation, the participant’s ability to reflect, and the participant’s ability to make themselves understood. The graph below shows that only one participant (A1) did not benefit from the visual method. She had poor eyesight, which strongly indicates that visual support compensates the difficulties that people with dementia have.
The report also concludes that the Talking Mats framework increases the interviewer’s ability to detect and compensate for some of the communication difficulties. Finally, it seemed that several of the participants have been able to learn how to use Talking Mats in the process.
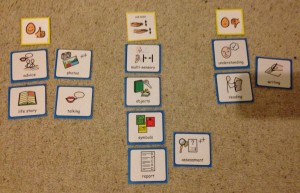
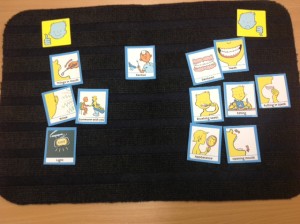
The photo underneath shows a Talking Mat conversation from the project. This Talking Mat gives an insight into how this person feels about what information is important to her, and what isn’t. It is in some way a difficult and abstract question, but most of the participants managed to both understand, reflect and answer the question when we used the Talking Mats framework.
Important information to this participant is information about new neighbours, the menu at the residential care home, economy etc. Less important is news about the Danish royal family, technology, getting older etc. Politics is definitely not important to her.
One of the issues which has emerged from previous Talking Mats and dementia projects is that many people with dementia experience difficulties with mealtimes and that it can affect people at any stage of dementia.
Mealtimes involve two of our most fundamental human needs, the basic physiological requirements for food and drink and interpersonal involvement. Mealtimes are particularly important for people with dementia as they may develop difficulties both with eating as a source of nourishment and with the social aspects of mealtimes.
In 2015 Joan Murphy and James McKillop carried out a project, funded by the Miss EC Hendry Charitable Trust, to gather information from the first-hand experience of people with dementia about their views about mealtimes. We ran three focus groups and used the Talking Mats Eating and Drinking Resource to allow participants to reflect, express and share their views.
Findings:
The people who took part in this study felt that there were significant changes in their eating and drinking since their diagnosis of dementia. For some, their experience of mealtimes had changed and several said that they now skip breakfast and sometimes lunch. For some this seemed to be related to forgetting to eat and drink, for others it related to changes in taste whereas for others these meals seemed to be simply less important. Forgetting to eat was particularly noted by the participants with dementia and confirmed by their spouses.
The social aspect of eating and drinking also changed for many of the participants and, given the importance of social engagement for quality of life it is important to be aware of the effects of changes in eating and drinking on mealtime dynamics. For some it may be that they are now less interested in the social aspect of eating with others at home. Others found it hard to eat out because of distractions and lack of familiarity while some felt embarrassed about eating out in front of strangers. Others still really enjoyed going out for meals but added that they preferred to go somewhere well-known to them. The shared mealtime may be a particularly crucial opportunity for social engagement as it plays a central role in our daily lives. Social relationships are central for not only enhancing quality of life, but also for preventing ill health and decreasing mortality (Maher, 2013).
Almost all the participants talked about how their taste had changed both for food and drink which in turn affected their appetite. Some families had overcome the problem of lack of taste by going for more strongly flavoured food. When asked specifically about drinking, thirst was noted as a significant change since diagnosis
Their feelings about the texture of food did not appear to have changed significantly and was simply a matter of preference.
Three additional health issues which the participants felt were connected with eating and drinking were poorer energy levels than before their diagnosis, reduction in ability to concentrate and changes in sleep patterns.
For a copy of the full report please click here Dementia and Mealtimes – final report 2015
We are very grateful to David Brennan, a Dementia Support Worker from Ayrshire for this powerful blog.
Over the years our service has supported many people with a diagnosis of Dementia, now and then we encounter individuals whose cognitive difficulties have greatly affected their ability to communicate. This can (in some cases) result in distress for the services user and their families, distress that could be reduced or even avoided if the individual had a way of being understood by those around them.
As a service we welcomed the opportunity to engage in the Talking Mats Training and as a Dementia Support Worker I was eager to have a tool that could help me overcome communication obstacles, having experienced situations where those I support become so frustrated because they desperately want to relay a piece of information, but simply cannot find the words to express themselves.
I saw talking Mats as a communication system for those who struggle with speech. However, after using the practice in a practical environment I realise that I have had underestimated its potential, for it has much wider applications in our role.
My first experience of using Talking Mats was when producing the video for the second training session. I enlisted the help of a gentleman from the neighbouring Day Care centre.
We had never met prior to the session. The Gentleman had no communication difficulties that I was aware of.
Using the Talking Mats acted as an instant ice breaker, giving two complete strangers a reason to sit down and interact together, quickly striking up a rapport. The Gentleman appeared at ease and was happy to talk in detail about the tiles for the chosen subject of ‘Leisure Activities’
The activity revealed more than expected though. Through the course of the conversation he voiced feelings on things he was perhaps not happy with. I discovered he was unhappy that he did not get out in the open air enough due to poor mobility and that he would have preferred to see musicians coming into his Day Care Centre. This was crucial feedback
It occurred that Talking Mats also had an effective use in the assessment and quality assurance process that exist within services, providing crucial feedback for continued person-centred planning.
Taking this on board I considered examples of service users within my current caseload where the activity could prove beneficial.
I have been working with one gentleman for many months. He could be described as a Man’s man, someone who often replies to attempts at conversation with short responses, even when speaking with his wife. He may struggle to remember the names of people and places but he typically has little other difficulty in communicating.
I attempted the same topic with this man. Much of the answers were as expected. He spoke about football and his favourite team, but the structure of the Talking Mats encouraged him to open up about some of the smaller details that until now he hadn’t felt the need to disclose.
In the most recent example I was asked to take part in a colleague’s Talking Mat video for her training. She is one of our newest members of staff and although we have already developed a good working relationship the activity allowed her more insight to the nature and history of her co-worker.
For my experience, as someone who can struggle with sensory stimulation, it allowed me to express some of my needs and obscure preferences (around the office and in general) in a safe environment where I felt able to communicate what would normally be very personal information. And to have someone listen and thoughtfully consider this was a rewarding experience too.
As a service, new to the Talking Mats system, we are just scratching the surface of how we can best implement this into our roles, but the possibilities are already multiplying at a rapid pace, almost as much as the benefits we are seeing.
David Brennan
Dementia Support Worker
Background
Social workers are required to complete a detailed assessment of their client’s needs. It is recognised that it can be a challenge to ensure clients fully participate in the process if they have cognitive or communication difficulties. The City of Edinburgh Council were keen to explore if we could adapt their standardized assessment tool and make it into a Talking Mat framework. Several staff in the council are already skilled practitioners in Talking Mats so are familiar with the framework and use Talking Mats in their practice. They are enthusiastic about the benefits of using Talking Mats both in terms of how it increases participation of service users but also because in their view it makes interviews easier for staff to undertake.
Structuring Talking Mats assessment framework
In order to develop the bespoke Talking Mat we held a seminar to discuss the social work assessment tool and approach used. Six key staff attended the seminar, facilitated by two Talking Mats associates. The discussion at the seminar identified a structure that would enable us to construct a coherent visual conversation that would cover the issues required to complete the assessment, using mind mapping to support this process. It is also important to identify a top scale that matches the question you are asking and make sure the options you are including are neutral and not leading.
The structure that emerged from this discussion is a Talking Mat that enables people to explore their views on 3 topics
- their home
- their health and well being
- their community involvement
Trialling the Talking Mats framework
Talking Mats then took the mind maps and developed these into symbol sets that were piloted by social work staff. At the end of the pilot a review was held and changes made which included alterations to
- the language used
- the symbols used
- the topic an option was included under
- making it clearer to staff when options were more abstract and required further explanation and or personalisation
Nicki Ewing from Edinburgh City Council who leads on the project says ‘ I am very excited that staff have a tool that can make assessment more meaningful for service users to participate in and makes it easier for staff to get good quality information’.
Next steps
We are thinking of holding a focus group for others that might be interested in using the framework for their practice if, you are interested please contact Lois via the info@talkingmats.com email – call your email ‘social work focus group’.
To mark Dementia Awareness week the Talking Mats team is keen to provide family training for relatives who care for someone with a communication difficulty.
Thanks to a generous donation from Miss Hendry Charitable Trust and support from Alzheimer Scotland, training has been carried out with family members at the Clydebank Alzheimer Scotland Resource Centre. Eight people who care for a relative with dementia (6 caring for a spouse and 2 caring for a parent) and one member of staff attended. None of the participants knew about Talking Mats before the training. They all cared for people who had difficulty expressing themselves and several told the group about the frustrations and despair they sometimes felt.
The training was carried out over 2 sessions.
Session 1 included an explanation to the background and purpose of Talking Mats, a demonstration, watching and discussing DVD examples, hands on practice, discussion of topics to be used at home with their relative and planning for next session.
Each participant was given a set of materials and by the end of the day all participants had understood the principles involved in Talking Mats and had gained the skills required to use it with their relative. They all said how much they had enjoyed the day and how much they had gained from it. They all committed to trying it with their relative and to bringing back their views to the follow up session. Each participant was given a post-it note at the end of the day and was asked to write any comments- positive or negative about the day.
Some of the comments:
• This was a very positive course today. It has made me feel very hopeful about establishing a time of coherent dialogue with my mother – albeit in a focused way and also in providing a tool for her to communicate in a simple way, her own thoughts, Thank you.
• Informative, informal, surprising. I enjoyed the course and felt I had gained from it.
• Could be a useful tool. Can’t wait to try it with my wife. Thank you.
• The course was very informative and well worth the time spent. Talking Mats is a very simple idea which seems to be working very well. I’m looking forward to trying it out and hearing how the others coped and what the outcomes will be.
• This was a very informative day and hopefully gives us a great way of communicating to find out my husband’s views on subjects.
The participants were assured that they could get ongoing support by phone or email and the staff member at the resource offered to provide local support.
Six participants plus two staff came to the second session. The others were unable to attend due to their relative being unwell. We had lively and helpful discussions where each person shared their own personal stories of how they had used Talking Mats and what it meant for them.
Overall they felt that Talking Mats was a powerful and helpful tool and that it gave them quality time together with their relative with dementia. The following comments illustrate this:
– small changes made a big difference
– It gives me time to sit down and listen to him
– It slows you down which is needed with someone with dementia
– It helps me know where he is at the moment
– It showed my husband the things he CAN do rather than what he CAN’T do
Relatives found out some things about their partner that they didn’t know e.g. one person with dementia had revealed that they didn’t like having the radio on all the time; another had toothache which the partner was unaware of; another said that food had become tasteless and he no longer enjoyed mealtimes as a result. The relatives were all able to do something as a result to help the situations – e.g. reduce the background noise of the radio, make a dental appointment, add more spice to their cooking.
One couple now use Talking Mats every few days on a regular basis to help the person with dementia think about issues and compare his mood from week to week
– He always feels up after he’s done a Talking Mat
This couple had also given a demonstration of using Talking Mats to a family meeting at the resource centre
Overall the participants found Talking Mats very helpful although two felt it had not been successful. We discussed the reasons for this and the group were very supportive and suggested that the staff could help by introducing Talking Mats as a group activity at the resource centre where these two people could be included. The staff at the centre were also very positive and plan to use Talking Mats both with individual people and with groups.
Overall it was agreed that Talking Mats is a very useful tool both for individual families and for dementia centres. We discussed future plans for individuals and also for the centre. This included designing a Talking Mat to discuss football and another to allow the people with dementia who attend the centre to be involved in planning the centre’s new allotment.
We plan to continue our involvement with the Clydebank Resource Centre and are now in the middle of running the same course in other Dementia Resource Centres.
Anyone wishing further information about Talking Mats training for family members, please contact us at info@talkingmats.com
During a research project funded by the Joseph Rowntree Foundation in 2007, Joan Murphy and Cindy Gray developed the Dementia Communication Difficulties Scale (DCDS) to help identify the communication difficulties that a person with dementia might be having and therefore help carers and staff to understand these difficulties and therefore support the person with dementia. The scale comprises 13 statements that are based on existing definitions of the communication problems commonly experienced by people as dementia progresses (Kempler, 1995; Health Education Board for Scotland, 1996):
In early stage dementia, the person
- may have difficulty coming up with words
- may tend to digress and repeat themselves.
In moderate stage dementia, the person
- may find it hard to understand what is said to them, particularly when being given complex information
- may have difficulty maintaining a conversation topic without losing track
- may use semantically empty words (e.g. thing, stuff) in place of content words
- may be difficult to understand.
In late stage dementia, the person
- may make little sense
- may not be able to understand what is said to them, even when simple language is used
- may often repeat what other people have said to them
- may communicate mainly in non-verbal ways
The DCDS requires a third party who knows the person with dementia well (a paid carer or family member) to assess various aspects of their communication on a 5-option scale. People are asked to circle the option that most closely describes the person in question.
Each DCDS option is assigned a score: for example ‘Never’ = 0, ‘Sometimes’ = 1, ‘Often’ = 2, ‘Always’ or ‘Says too little for me to judge’ = 3. A person’s DCDS rating is obtained by totalling their scores for all 13 statements. DCDS ratings can therefore range from 0-39, with a higher rating indicating a greater degree of communication difficulty.
The following stages of dementia group definitions were produced:
• DCDS ratings between 0 and 10.5 = early stage
• DCDS ratings between 11 and 19.5 = moderate stage
• DCDS rating between 20 and 39= late stage.
The Dementia Communication Difficulties Scale is brief, straightforward and quick to complete, and may therefore provide a highly useful tool for the care staff, clinicians and practitioners involved in assessing the needs of people with dementia.
If you would like a copy of the scale please click here: Dementia Communication Difficulties Scale
References:
Kempler, D. (1995). Language Changes in Dementia of the Alzheimer Type. In R. Lubinski (Ed.), Dementia and Communication, San Diego: Singular Publishing Group.
Health Education Board for Scotland (1996). Coping with Dementia: A Handbook for Carers. HEBS.
Using Talking Mats with Tony, a 53 year old man with learning disability and dementia. A guest blog by Rebecca Leighton Specialist Speech and Language Therapist and Consultant for elenbi-uk
“When I change I will be different”
Tony was referred to me for Speech and Language Therapy around 6 months after being diagnosed with mixed dementia. Dementia was having many effects on him but a key impact was communication difficulties: one of these difficulties was dysarthria (for him, this meant slow, slurred, effortful speech and difficulty maintaining enough breath support to finish his sentences) and another word-finding problems (difficulty remembering and producing the words he wanted to say – like the “tip of your tongue” phenomenon we all get from time to time, but occurring in most of Tony’s sentences). These two communication difficulties combined made talking very tiring and frustrating for him.
When I first met Tony, one of my aims was to find out what he wanted to achieve with Speech and Language Therapy. We discussed this but it was tiring for Tony and it became clear very quickly that using words alone was not helpful. It also became clear in that first session that although Tony was concerned about his speech, he was more concerned about his future and other areas of his life. He was worried about how he would enjoy life with dementia. He knew he would get worse and he wanted to know how he and his family would cope with that. Tony said “When I change I will be different. What will I do with myself?”
I introduced Talking Mats to Tony at our next session, suggesting that it would be a way of exploring what he was worried about in terms of his overall health and wellbeing and also what he might want from Speech and Language Therapy. We did four Mats over the course of two sessions:
Mat 1: Starter topic (food). Tony managed a three-point scale easily (“like” “dislike” and “not sure”) and told me “This is alright, its easy. I can talk if I want. But I don’t have to.”
Mat 2: “My worries”. Tony used a three point scale to indicate whether he was “not worried”, “a bit worried” or “very worried” about a range of aspects of his life and future. We found that Tony’s main worry was what he would do with his time as his dementia progressed.
Mat 3: “Activities with dementia” – a sub-mat based on Tony’s main worry identified in Mat 2. This was done jointly with his advisor, Sabira, from his local dementia support service, who planned the mat with me to ensure it covered all the options Tony had available to him locally. The mat revealed that Tony was already attending a well-being café but wanted to try other well-being cafes too, to meet more people. He was keen to try the singing group and also felt that his family needed support. Sabira commented that she thought Talking Mats should be used more with people with dementia and she intended to explore this within her own service.
Mat 4: “What I want help with from Speech and Language Therapy”. Again we used a three point scale, this time to indicate “yes”, “no” and “maybe” to possible goals for Tony. Options included assessment, therapy and advice. We chatted around each topic, giving Tony more information on each possibility and discussing if and how it could benefit him. Tony made informed choices around each option, and made the decision to start by creating a Life Story.
With Talking Mats, Tony has been able to give his full views on some very difficult topics for him. He has done so in a way which has reduced the demand on his speech, which made the discussion easier and less tiring for him. He has taken control of his Speech and Language Therapy care and has made informed decisions about his therapy goals. Perhaps more importantly he has taken control of his future and made informed choices about what he wants for himself and his family for the rest of his life.
Talking Mats could be used by many services for people with dementia. Imagine how empowered people with dementia would be, for example, if their social worker or dementia adviser were able to use Talking Mats with them to identify their needs and wishes and help them choose what they want for their present and future. What better way to involve people in their own care?
The only caveat? Get in there early. Empower people to tell their story while they are still able to use pictures and words to do so. Dementia can steal these skills, burdening families with making decisions on behalf of their loved ones. As a daughter, mother, wife and sister myself, I know I would feel much more at ease with making a decision for my relative with prior knowledge of what they themselves would have wanted. Talking Mats is one way of finding that out.
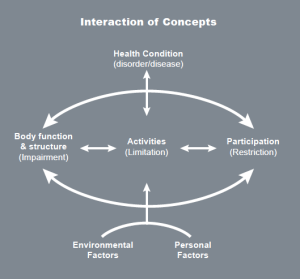
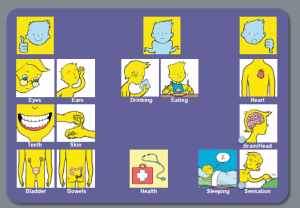
The Health and Well-being resource is based on the WHO International Classification of Functioning, Disability and Health (ICF) which is a framework which covers almost every aspect of daily life and can be applied over different cultures (WHO 2001).
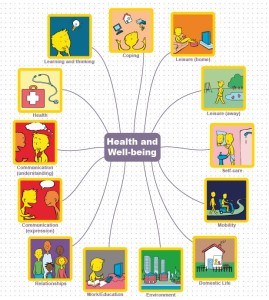
Use of the WHO ICF helps professionals to think holistically about the people they are working with. We have produced four sets of symbols, based on WHO ICF, to help people express their views about different aspects of their lives. These cover 13 topics:
You can use the symbols in different ways, depending on the cognitive abilities of the person you are working with. For example, if you are working with someone who can understand abstract concepts, you could start with the 13 main health and well-being symbols. Your top scale might be ‘managing’ and ‘not managing’. Here is an example of a mat completed by Duncan who had a stroke which affected his ability to communicate through speech:
Using these symbols as a starting point, Duncan could tell us that his main concerns related to worries about his health, expressive communication and work. From here, we did ‘sub mats’ to help Duncan identify the specific areas he wanted to work on/explore.
Here is the mat Duncan completed in relation to his health:
Having done this mat with Duncan, it became clear that he was worried about various aspects of his health, particularly the risk of having another stroke. The wider team were able to give him and his wife information about stroke prevention. Other mats were also completed, exploring expressive communication, work and education and higher level communication (which is included in the ‘learning and thinking’ topic, and covers written communication as well as memory and concentration). Using the Health and Well-being symbols, we were able to work with Duncan to help him identify the main issues that he wanted to work on and then work towards more specific rehabilitation goals. Duncan had copies of all the mats he had completed and found it useful to refer to them over the months. This helped everybody stay on track in relation to his goals and he was also able to track his progress over time.
Have a look at our Health and Well-being resource on our website. It is available both as an original Talking Mat with a physical mat and symbol cards or as a digital version as part of The Talking Mats pro subscription
Not many people enjoy going to the dentist but it can be a real problem for people with communication disabilities.
Recently I wrote about using Talking Mats in a care home to find out the views of an elderly lady with communication difficulties and dementia who had lost her dentures. click here. Using the mats, she was able to tell us that she was unwilling to open her mouth but thought that if someone was with her she might manage better.
Following our Talking Mats conversation the Care Home arranged an appointment with the dentist for the following week. Her son went back over what we had talked about just before the visit. She managed fine, opened her mouth and her treatment was carried out successfully.
Dentistry is a huge problem for many people, but the impact of not being able to cooperate can have serious implications for a person’s appearance, comfort, quality of life and health.
In preparing for a visit to the dentist it’s important that the person understands both what is going to happen and why its happening. Talking Mats is a visual tool that can help the person with communication difficulties both with understanding and also expressing their views. In this way the family and carers can find ways to reassure the person and support them to get the appropriate dental treatment.
Please let us know your thoughts on supporting people in similar situations.
 Online training login
Online training login