Talking mats are delighted to announce the new Talking Mats ’ Sexual health and relationships’ advanced seminar and resource which is now available to book.
Resource background and development
This resource has been developed in partnership with the REACH team in Perth and Kinross council. In her blog Let’s talk about sex: part one Julia Pollock, a speech and language therapist with this multidisciplinary team describes why this resource is much needed and how it has helped open up discussions on a subject that otherwise might be more challenging. Her second blog Let’s talk about sex: part two describes the impact that this talking mats resource has had on one young person as they navigate their way through the criminal justice system and their sexual development from childhood to adult hood’
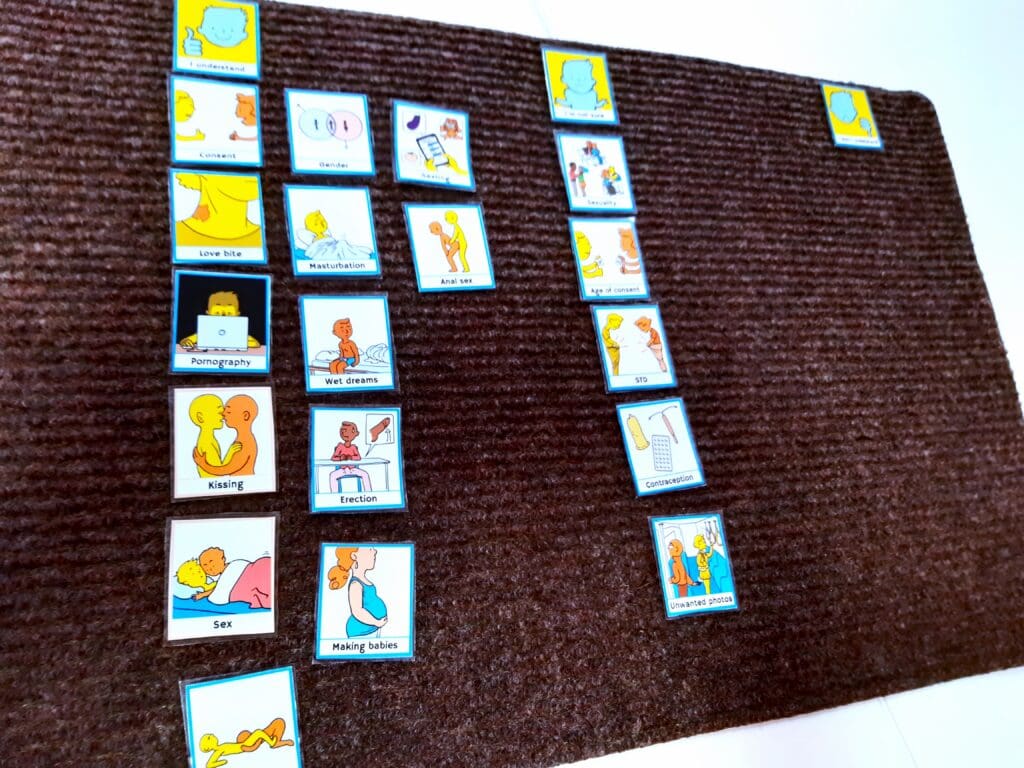
What is in the Talking Mats Sexual health and relationships resource ?
The resource has three topics:
- Sexual knowledge. This topic allows practitioners to explore what young people know. It also includes a sub mat of body parts to be used if more concrete options are required
- Being close. This topic explores the young person’s view of intimacy. It can be used to explore what they have experienced in relationships and or what they want.
- Sexual interests. This topic grew out of the Reach team’s focus on working with young people at risk of being involved in harmful sexual behaviour so it is to be used with care and is not appropriate for all thinkers. The options need to be personalised carefully.

Using this resource
From our piloting and testing phase this Talking Mats sexual health and relationship resource has been found to be very helpful for those working in this field but, it needs to be used with sensitivity and care. The options and images that we have developed are clear but are sometimes explicit. It is for this reason that this resource is not going to be available on our digital platform. It is important that practitioners using the resource are aware of the issues and think carefully about which topics and options are helpful for the young person they are working with before presenting them. Practitioners using this resource need to work in a context that enables the young person to access any ongoing support for issues that may arise.
Accessing this resource
To access this resource, you need to:
- Have completed the Talking Mats foundation course.
- Be familiar with your organisation’s child protection and adult support and protection procedures
- Be clear about why you are using this resource and for what purpose for example to explore sexual relationships in general or to open up discussions about harmful sexual behaviour. You need to be experienced enough to be able to adapt the resource for those different contexts.
- Book onto our advanced seminar which we are hosting on the 18th of September 1:00 PM to 3:00 PM in conjunction with the REACH multidisciplinary team. This seminar allows for the context, challenges, risks and benefits of using the resource to be fully explained. This will include best practice examples and impact stories. It will give you the opportunity to explore the resource further and to ask any questions. The cost is £80 per participant and this covers the resource and the seminar.
Click here to book your place on this Advanced seminar. Places will be limited so make sure to book soon. Resources will be posted out the week before the seminar.
This week’s guest blog, the first of 2 from the authors (Lois Cameron, Nikky Steiner and Luccia Tullio), describes the development process of a set of symbols aimed at supporting practitioners to reflect on the role of identity within their practice.
Every person has their own unique identity, just like they have their own unique fingerprint.
Identity is about how we see ourselves and how the world sees us.
Background
The Royal College of Speech and Language conference 2021 was titled ‘breaking barriers and building better.’ Professor Harsha Kathard from the University of Cape Town gave the keynote presentation and reflected on the key role understanding identity has in clinical practise, stating that ‘understanding identity is key to inclusion’. Secondly, she stressed that if we want to develop better services and support then ‘Turning the gaze to reflect on our positionality is central to change’ .Ash R et al (2023) in their editorial for the British Medical Journal highlight how interventions normally focus on single categories of social identity and ‘fail to account for the combinations of, or intersections between, the multiple social characteristic that define an individual’s place in society.’ They argue that ‘systems of care may consequently overlook overlapping systems of discrimination and disadvantage and exacerbate and conceal health inequities.’
The Development group
Following feedback from clinicians and people who use Alternative and Augmentative Communication (AAC) a working group was formed in March 2021 to explore the role of identity, diversity, equality and inclusion with in AAC practice.
Communication Matters and AAC networks within the UK advertised the group and 12 people responded. These people came from a range of organisations and had a range of lived experiences of diversity including people who use a communication aid to help them communicate. The work was funded by the Central London Community Health Trust and Talking Mats Ltd facilitated the meetings and the work
The group worked shaped the resource by reaching a consensus about the components of life that contributed to identity. In the end the group agreed on gender, sexuality, disability, race, neurodiversity, culture, family structure, voice, bilingualism, religion, mental health, personality, politics, intimacy, connecting with others and occupation. The process of developing the symbols was hugely helpful in unpicking what was actually meant by the various aspects e.g. voice. The original image for voice represented accents but the group discussion shaped the image to represent much more so the final image included a rainbow flag, a more general sound wave to represent tone, a Spanish word and an image to represent disability. As one group member said ‘my cerebral palsy is part of my identity. If I am having a voice I want to reflect that identity – I want a cerebral palsy voice’. Identity and the issues surrounding it can be emotive but the focus on the symbols helped contain the emotion and supported group members to listen to the perspective of others.
The whole iterative process of developing the resource and clarifying what the symbols should look like allowed the group to be clear about the individual meanings of abstract topics. This wider understanding was captured in a glossary to go alongside the symbols. For example, Identity has the following definition: Every person has their own unique identity, just like they have their own unique fingerprint. Lots of different characteristics make up our identity. This is what makes us different from other people. Sometimes we may share some of these characteristics with other groups of people, which can also be part of our identity. Identity is about how we see ourselves and how the world sees us.
Equality, Diversity and Inclusion: a visual framework to support the exploration of Identity within practice.
The resource is seen as a support for constructive reflection by practitioners on identity and allows them to consider the different aspects of their patients’ lives that may impact on their interventions. The final Talking Mats symbols have the suggested top scale of ‘I considered a lot’, ‘I considered a bit’, ‘I have not considered yet ‘. It could be used individually or by a team as a group discussion tool.
As the resource uses the Talking Mats framework, it is recommended that practitioners have completed their Talking Mats foundation level training
If you are interested in completing Talking Mats Foundation Training, you can see the training options in our shop here.
References
Kashard H 2021 Keynote breaking barriers and building better The Royal College of Speech and Language conference.
Ash Routen, 1 Helen-Maria Lekas, 2 Julian Harrison, 3 Kamlesh Khunti1,2023 Interesectionality in health equity research BMJ 2003 https://www.bmj.com/content/383/bmj.p2953
Our thanks for this blog go to Olivia Ince, Talking Mats Licenced Trainer and Speech & Language Therapist. This blog post reflects on the use of a Talking Mat with a Thinker called M who speaks English as an additional language. The Listener in this Talking Mat is Jono Thorne who is a colleague of Olivia. Jono did this Talking Mat for his video as part of a Foundation Training course run by Olivia.
M is a young adult who came to the UK as an unaccompanied asylum-seeking child. M is from a country in Central Africa and speaks a language which is not widely spoken outside of the region. Accessing interpreting and translation services in the UK for their native language is very difficult and M has therefore had difficulties learning English. This means the people around M often have difficulties finding out M’s views, which is why Jono thought a Talking Mat could be an invaluable communication tool for M.
M already uses some visual support, for example hand gestures and using objects such as food items when having a conversation in the kitchen. The people around M are unsure what M’s level of comprehension is in English and therefore they make adaptions such as simplifying their language. M’s expressive language in English is typically the use of one- or two-word utterances and yes/no responses.
To see if M would be able to engage with the Talking Mat process, Jono chose a simple topic to start with and one which he knew would interest M: food. The Top Scale used was like/unsure/ don’t like. Jono noted that M quickly understood the concept of the Talking Mat and the visual element seemed to support M’s understanding. The Talking Mat process including the side-by-side listening also facilitated rapport building.

Jono noticed that M was decisive and seemed certain about their placement of the option cards. The Talking Mat helped M to share their views on a larger number of items than would likely have been possible via a verbal conversation. M also joined in with the recap of their Talking Mat as part of the review and reflect by reading out the Option cards with Jono, which meant M was even more involved with the process.
There were a couple of difficulties for M during the Talking Mat process: the blanks and the option to change where the Option cards were placed. Jono tried to explain these steps using simple language but M did not appear to understand these concepts due to their level of comprehension of English. As M had seemed sure of their initial placement of the Option cards and they joined in with the recap, Jono felt that the Talking Mat was an accurate reflection of M’s views that day. Continuing to model these steps to M will likely help them to develop their understanding of these parts of the Talking Mats process over time.
Jono reflected on how useful it was to now know which foods M likes and doesn’t like. He also reflected on the potential future use of Talking Mats with M on more complex topics and to facilitate participation in decision-making now that it’s clear M understands how a Talking Mat works.
If you are interested in completing Talking Mat Foundation Training, you can read more about it here.
We are pleased to share a new blog from Talking Mat Associate, Jess Lane, as part of a 2-part series on the use of Talking Mats within Child and Adolescent Mental Health Services (CAMHS).
In Part 1, Jess described how Talking Mats can provide children with a safe space to explore topics that they might otherwise feel unable to communicate about, in a way that is highly supportive, sensitive and impactful. Check it out here:
In Part 2, Jess reflects on the use of Talking Mats by all members of the multidisciplinary team. We also hear from Nikki Low, Specialist Occupational Therapist, who reflects on her use of Talking Mats in the acute mental health setting.
Later in the blog, Jess explores how Talking Mats can be used as part of a post-diagnostic package of support for autistic children to support more focussed, strengths-based conversations, in line with the core principles of neurodiversity affirming practice.
A Multidisciplinary Approach
Welcome back to my 2-part series on the use of Talking Mats within CAMHS. In Part 1, I described how the implementation of Talking Mats by all members of the multidisciplinary team has transformed the way children are supported in the acute mental health setting. I have since reflected with clinicians from across Speech and Language Therapy, Nursing, Psychiatry, Dietetics, Occupational Therapy, Physiotherapy and Psychology on how Talking Mats continue to be used on CIPU to facilitate the direct and meaningful involvement of children in care planning, and to facilitate equity of access to therapeutic intervention.
Nikki Low reflects on using Talking Mats in her role as a Specialist Occupational Therapist:
“I am a Specialist Occupational Therapist working in a Psychiatric Inpatient Unit with children under 12, many of whom, in addition to their mental illness, have an intellectual disability, are neurodivergent and/or have experienced complex trauma. This can make meaningful interactions about thoughts and feelings challenging or even impossible, particularly when discussing sensitive topics.
We strive to provide a client centred approach to care and treatment for our young patients but this can be difficult when they are unable to express themselves. Talking Mats has revolutionised our approach with these children. It has proven to be a powerful tool, transforming communication experiences for individuals of all abilities. I have used Talking Mats to engage patients in assessments and to formulate their treatment goals. Its user-friendly design, customisable features and positive impact make it an invaluable resource in the care and treatment of our vulnerable young patients.
As a unit, we have rolled out training to all core staff in order that we can incorporate Talking Mats into our practice. By doing this, we have been able to facilitate more inclusive and person-centred interactions, ultimately fostering a more supportive and empowering environment for all involved.”
Implementing Talking Mats across a whole staff team has increased the capacity and capability of clinicians to routinely involve children in decisions pertaining to their care. It has also contributed to a culture whereby Talking Mats are considered at each stage of a child’s admission, to support assessments of capacity and mental state, medication reviews, engagement with advocacy services and participation in all multidisciplinary team meetings and case conferences.
Post-Diagnostic Support
Most recently, I have used Talking Mats as part of a post-diagnostic package of support for autistic children, to support more focussed, strengths-based conversations around what it means to be autistic. This has involved developing a symbol set based on SIGN guidelines and associated resources, to support children who have recently been diagnosed as autistic, to engage in a conversation about what would be helpful for them to know.
When presented with a Top Scale of Helpful, Not Sure, Not Helpful, children were able to share their opinion on a range of options, including (but not limited to): facts and figures, autistic famous people, links to other work, skills, strategies and resources. An example is provided below. From this, I was able to create a personalised information pack for each child, based on what they would (and would not) find helpful to know about autism.

Most children shared that it would be helpful to find out about autistic famous people. This provided the foundation for a follow-up conversation about identity. Some children shared that they would find it helpful to find out about incidence and prevalence figures. Others did not. This was reflected in their information packs. For children who shared that they would like to understand how being autistic might impact, or otherwise feed into, therapeutic work for anxiety, I worked with colleagues from across Psychology and Nursing to ensure this was accurately reflected in their information packs.
Using a Talking Mat to scaffold conversations about what it means to be autistic has been well received by other clinicians involved in providing post-diagnostic support. By providing children with an opportunity to identify exactly what they would like to know about autism, clinicians have been able prioritise areas of support and signpost to the most relevant resources. This speaks to legislation that calls for the greater involvement of patients in decision making, in line with the mantra: no decision about me, without me.
Anecdotally, I have found that using Talking Mats as part of a post-diagnostic package of support has made a significant contribution to the development of a more streamlined, relevant and person-centred approach to sharing information. Using Talking Mats in this way has provided children with a dedicated space to voice their opinion on a topic that they might not have previously inputted into, that has been actively listened to and directly acted upon.
It is hoped that in sharing how Talking Mats can be used as part of a post-diagnostic package of support, this blog might encourage others to consider how they might achieve similarly positive outcomes for children with other diagnoses. If you have used Talking Mats as part of a post-diagnostic package of support for children or adults, I would love to hear from you! Please do get in touch at info@talkingmats.com.
Our thanks for this blog go to Deborah Little, Speech and Language Therapist; Clinical Lead for AAC & Total Communication (Children and Young People) NHS Dumfries and Galloway.
“Can we do a Talking Mat today Deborah? This is the question I am asked as soon as I enter the Learning Centre in one of our local schools by an enthusiastic 8 year old who has been exploring what completing a Talking Mat (TM) is all about this term. While we are in the early stage of this school’s TMs journey, the impact of embedding the approach into the fabric of how Children and Young People (CYP) are supported to communicate in school is already proving transformative.
Article 12 of The United Nations Convention on the Rights of the Child (UNCRC) guarantees children the right to express their views and opinions freely in all matters affecting them. The responsibility of ensuring children experience this right is also underlined in NICE guidelines (2022) that state: “Education, health and social care practitioners should always: put the life goals and ambitions and preferences of the disabled child or young person with severe complex needs at the centre of planning and decision making.”
Working with my teaching colleagues within one Additional Support Needs (ASN) setting this year, we reflected on how effectively the CYP were able to give their views and how consistently these views were acted upon in meaningful ways. We felt that this was an area we really wanted to improve upon and specifically we wanted to explore the following key questions in our minds:
- How can we support CYP’s understanding of their right to give their views and opinions? We reflected that for some CYP, their experience of being able to do this was very limited and that their understanding of using a TM was not yet at a stage where they were able to represent their views. We therefore wanted to prioritise finding out what helped these CYP to use TMs with understanding.
- How can we support CYP to know that they can tell us they aren’t happy about something? We reflected that during ‘Emotions Works’ discussion times many of the CYP routinely shared that they felt ‘happy.’ It was rare for the CYP to talk about unhappy feelings. We felt worried that the CYP often gave responses that they felt would be ‘right’ or pleasing to adults.
- How can we ensure we create a culture of prioritising time and space for CYP to share their views, opinions and ideas? We thought about opportunities throughout the school week that would create space and motivation for the CYP to engage with TMs. We wanted to achieve a feeling of TMs being integral to the everyday, as opposed to a sporadic ‘add on.’
To answer these questions, we agreed on the following key change ideas to implement and evaluate:
Developing understanding of the Talking Mats process linked with familiar learning opportunities.

Dynamic Assessment is an approach familiar to those working with CYP who use Augmentative and Alternative Communication (AAC). Adapting activities dynamically, being responsive to CYP’s progress, allows progressive skill enablement. Together with teaching colleagues, we applied this thinking to helping the children use TMs with understanding. If we had tried having a conversation using TM only a couple of times, our evaluation could have been that TMs wasn’t yet a tool we could use because for example, the CYP were putting all their symbols into the ‘I’m happy with this’ column only. Instead, we thought “OK, that’s where the CYP are now, let’s give them opportunities to practise engaging with this new tool and time to develop using the approach with understanding.” Put another way, we prioritised another key concept within the field of AAC: we Presumed Competence. We believed that the CYP had the ability to share their thoughts, feelings and ideas if we introduced TMs gradually, linking with the activities above, that were tangible and familiar to the thinkers.
Consciously modelling that is OK to have negative feelings and opinions.
When a CYP is learning what might be possible in terms of communicating with AAC, best practise is for supporting adults to model the AAC. This means, adults ‘use AAC to teach AAC.’ We show CYP that we highly value the AAC and want to use it too. We use it in real situations, modelling vocabulary to help CYP understand the symbolic vocabulary and how they can begin to use it too. When helping the CYP understand how TMs could help them express a wider range of emotions, we tried out using this approach. Now and again, supporting adults would share with the CYP how they were feeling about things using TMs and would include negative feelings.

One CYP had a memorable response to my sharing that I was feeling “not happy” with my cat. The CYP’s eyes widened and he became instantly animated, using his AAC to ask “cat..bad..what?” I was able to explain that my cat had been scratching my carpets and I was feeling upset about this. The CYP then used his AAC to say “cat…dig!” He pointed at the ‘not happy’ symbol in the Talking Mats top scale, jointly sharing his attention to this symbol and understanding of what this meant with me. The next week, we used TMs to ask this young person about a social group he had attended. For the first time, we noticed him ‘swithering’ across his top scale while making his choices. Also for the first time, I was confident that he shared his authentic feelings with me. I reflected on the power of modelling and normalising feelings that are ‘not happy.’
So, where are we now? The key themes from our findings after a year of using TMs as described above are:

In summary, using TMs in this setting has all supporting practitioners in agreement that it is not only important to listen to CYP when we know they might be having a tough time; we need to create space to listen all of the time, week to week, with authenticity and without agenda. The principles regularly used within AAC practice of: modelling, presuming competence and dynamic assessment have been effective in supporting more children to be able to experience their UNCRC Article 12 Right, more of the time and with increased understanding and confidence.
References
- UN Convention on the Rights of the Child – UNICEF UK
- NICE Guidelines [NG213] (2022) Disabled Children and Young People up to age 25 with severe complex needs: integrated service delivery and organisation across health, social care and education.
- Emotion Works www.emotionsworks.org.uk
- Daneshfar, S and Moharami, M (2018) Dynamic Assessment in Vygotsky’s Socioculturaly Theory: Origins and Main Concepts. Journal of Language Teaching and Research 9(3):600
- Donnellan, A (1984) The Criterion of the Least Dangerous Assumption. Behavioural Disorders, 9 (2), 141-150
- Sennott, Light and McNaughton (2016) AAC Modelling Intervention Research Review. Research and Practice for Persons with Severe Disabilties 41 (2)
Talking Mats is available both as a physical resource and as a digital web-app. In this blog, our Digital Lead, Mark, gives an update on some exciting recent developments on our Digital Talking Mats platform.
It’s been over 2 years since we launched our new Digital Talking Mats platform, and we’re so pleased that more and more of the Talking Mats community continue to discover how it can be used to improve conversations in a wide range of contexts and situations.
We’re always looking for ways to improve the user experience of Digital Talking Mats, and over the last couple of years we have so appreciated the feedback given by Talking Mats customers who have been using the platform.
This feedback has led to plenty of tweaks and updates behind the scenes, but in this blog I want to highlight some updates we have recently implemented, which we hope will improve the experience for those using our digital platform, and also let you know about what upcoming features are in the pipeline.
Grouping and Deleting Thinkers
Users can now create groups/categories for their Thinkers, and organise them in a way that is most helpful for their context. Whether it is school classes, hospital wards, or care homes, for example, users can choose what to name the groups, and how many Thinkers are in each group.

As well as creating Thinker groups, users now have the option to delete any Thinker from their list. This may be a former patient, a Thinker from a previous job, or simply a Thinker that was used to test out the digital platform.
Sharing Personalised Mats
For users who are Talking Mats trained and are part of a Digital Talking Mats Organisational Subscription, we’re excited to say that personalised Mats that have been created can be shared with other members of your organisation. This means that if you work in a specialist department and require a bespoke mat for your context, one member of your department can create a personalised Mat, and share with every member on the subscription.

Upcoming Feature: Private Resources
At Talking Mats, we often do consultancy projects with organisations, to create specialist Resources for specific contexts. Sometimes these Resources end up for sale in our shop, for example, our Funeral Planning, Careers, Work & Employment, and Youth Justice Resources.
In other cases, an organisation may wish to have exclusive access to a Talking Mats Resource produced as part of a consultancy. This is easily achieved with physical resources, but has so far not been possible in the context of the digital platform. With the upcoming private resources feature, we will be able to upload a resource and grant access only to a specific organisation.
At Talking Mats, we are committed to continually developing and improving our digital product for customers. If you have any feedback, or any ideas for improvements we can explore in the future, please get in touch with us at info@talkingmats.com.
If you are interested in Digital Talking Mats for yourself or your organisation, you can read more about the platform here. We have subscriptions available from as little as £5 per month and you can see the available options in our shop here.
Do you work with people with intellectual disabilities and / or autism?
Researchers at the University of Hertfordshire have been working with Talking Mats to develop a range of symbols to help people with intellectual disabilities and/or autism to communicate symptoms of long Covid. It is hoped that these symbols will help facilitate conversations and improve accessibility to long Covid service pathways and improve health outcomes.
There are three topics that have been developed:
- Symptoms – This Topic uses a suggested Top Scale of I have / I sometimes have / I don’t have. Options in this topic include heart going fast , dizziness , brain fog.
- Mood – This Topic uses a suggested Top Scale of This is me / This is sometimes me / This not me. Options in this topic include frustrated, not interested, confident
- Getting Help – This Topic supports you to discuss how supported the individual feels and where their key supports are coming from. A suggested Top Scale is Going well / Unsure / Not going well. Options in this Topic include GP, online/phone support, specialist team.
This Talking Mats resource was developed in partnership with a group of people with intellectual disabilities and people with autism alongside a range of health professionals. People who had lived experience of long Covid were also involved in the group.
Participate and use the resource
We would like to hear from a wider cohort of practitioners working with people who have learning disabilities. For example, nurses, speech and language therapists and occupational therapists. We want to know if there is a need for this long Covid Talking Mats resource. This resource can also be used where long Covid has not been formally diagnosed but you want to listen to the person with a learning disability and hear about their experience of their long-term health condition.
If you would like to participate, and meet the following criteria, we would love to hear from you.
Criteria:
1. Have completed Talking Mats Foundation Training course.
2. Work in a setting supporting people with intellectual disabilities and/or autism.
If you would like to get involved, please complete the following survey by the end of April 2024.
Click here for the Long Covid Survey
Please note that should you consent to be involved in this project, your information will be shared with the University of Hertfordshire.
The team will be looking for feedback by the end of July 2024 and you will be asked to fill in a short survey for each Talking Mat that you complete . This survey will be sent to you alongside the long Covid resource.
If you have any questions about this, please do not hesitate to contact info@talkingmats.com
Talking Mats is delighted to welcome a new Training Associate, Jess Lane. Jess has written this blog to introduce herself to the Talking Mats community. Welcome, Jess, we’re thrilled to have you as part of team TM!
Hello! My name is Jess and I am thrilled to be introducing myself as a newly appointed Training Associate for Talking Mats.
About Me
I am a Specialist Speech and Language Therapist with a clinical background in Learning Disabilities and Paediatric Mental Health. I also work for the Royal College of Speech and Language Therapists (RCSLT) as a Research and Outcomes Officer, where I help to build research capacity, capability and culture within the profession. I am currently studying towards a Clinical Doctorate in Professional Health Studies, looking at the use of Talking Mats for facilitating the direct and meaningful involvement of children in care planning.
Talking Mats has been a huge part of my career to date. This began in my hometown of Gloucester, where I worked as an SLT in an Intensive Support Service for children and adults with learning disabilities. Changes in my personal circumstances saw me relocate to Scotland in 2022, where I worked across Specialist Child and Adolescent Mental Health (CAMHS) Services in and around Glasgow. Most recently, I worked at a National Child Inpatient Psychiatric Unit (CIPU), supporting children with severe and enduring mental illnesses.
Talking Mats in CAMHS
Since completing my Licenced Training last year, I have been working with Talking Mats to deliver Foundation Training for CAMHS teams across the UK, as well as driving an upskilling initiative for Specialist Children’s Services locally in Glasgow. I have found that Talking Mats provides children with a safe space to explore topics that they might otherwise feel unable to communicate about, in a way that is highly supportive, sensitive and impactful. This is encompassed by feedback from a recent patient, who wanted to share that “using a Talking Mat is easier than talking because talking about how you feel can be difficult”.
Many of the children admitted to CIPU present with transient communication difficulties that can exacerbate the impact of mental ill health. Some children present with underlying communication difficulties that were not apparent in the community setting. Other children do not present with communication difficulties, but find it extremely difficult to think about, or share their views on, sensitive topics. Because of this, Talking Mats have been used extensively by the multidisciplinary team on CIPU to:
- Facilitate the direct involvement of patients in goal setting and care planning
- Adapt and extend traditional mental health inventions, including talking therapies
- Support capacity assessments, assessments of mental state and medication reviews
- Improve engagement with local advocacy services as part of the CTO process
- Adapt and extend assessments such as the Child Occupational Self-Assessment Tool
- Improve access to psychoeducation for patients with anxiety and/or depression
- Improve engagement with meal planning for patients with an eating disorder
- Support the differential diagnosis process for mental illnesses such as catatonia

Using Talking Mats in an acute mental health setting has transformed the way clinicians from across Nursing, Psychiatry, Dietetics, Occupational Therapy, Physiotherapy and Psychology engage with the children about their care and treatment. Feedback from the clinical team, children and their parents/carers has been overwhelmingly positive. Talking Mats are now used routinely on the unit to support children’s access to (and engagement with) therapeutic intervention as part of their wider recovery, as well as ahead of all multidisciplinary team meetings and case conferences to ensure each child’s voice is heard and acted upon.
I am so pleased to have joined the Talking Mats team and am very much looking forward to supporting other people to use Talking Mats in a range of settings. Stay tuned for a follow up blog on how I have used Talking Mats as part of a post-diagnostic package of support for autistic children and young people, designed to support more focussed, strengths-based conversations around what it means to be autistic, in line with the core principles of neurodiversity affirming practice.
Thanks to Julia Pollock, Highly Specialist Speech and Language Therapist (SLT) from the REACH team in Perth for the second part of this latest guest blog sharing information about our exciting project, which has aimed to produce a resource to open up conversations with young people about sex.
By far, the most impactful feedback we’ve had during the pilot stage of this project has come from the social worker of the young person who I initially created the resource for. She was very keen to share with us that she had used the resource with the young person (two years on) and said it was ‘absolutely fantastic – I can’t tell you how good it was’.
Using the updated version, she was able to revisit the young person’s sexual knowledge and understanding and found that he was able to understand and have adult discussions around much more complex and abstract concepts than he had previously. The concepts included consent, contraception and sexually transmitted diseases. This was in stark contrast to his initial bewilderment when we first introduced the resource to him!
This has been a perfect case study for us as the resource has been used to support this young person through their entire criminal justice journey and through their sexual development into adulthood. The first draft had been used to initially gather information about his sexual knowledge and understanding in addition to information about the harmful sexual behaviour. It was later used to guide and support his sex education.
Now we have come full circle, with social work using the updated version of the resource to reflect on the past, helping him to understand his sexual development and to help guide his understanding around navigating future adult relationships in a safe and appropriate way.
‘He is ‘a confident, happy young man with the knowledge he needs for the future. There has been a lot of repair to his sense of self and moving from describing himself as a “monster” to understanding that he had a lack of knowledge and didn’t have the skills to navigate his sexual development safely. He is now able to accept his sexual feelings as being a “normal” part of development and to think how these can be expressed safely. His ability to integrate knowledge/reflect has been remarkable!‘
‘Importantly, we have also worked hard with the family to help them to accept him developing into a young adult with sexual feelings and the need to have access to peer relationships.‘
‘The Mat was brilliant in bringing all this together and providing the scaffolding to have these discussions with him.’
As a speech and language therapist, this process has been such a fantastic learning experience. It has been a joy and a privilege to work together with our social work and Talking Mats colleagues to create what will hopefully become an invaluable and essential resource in this field.

We are looking forward to sharing more information about the project and resource in an Advanced Webinar for practitioners who have already completed Talking Mats Foundation Training, in September 2024.
Inspired to think about Talking Mats Foundation Training? Find out about all the options we have available here.
Talking about sensitive issues can be challenging at times. We are so excited to publish this guest blog from Julia Pollock, Highly Specialist Speech and Language Therapist (SLT) from the REACH team in Perth, Scotland, explaining how a newly developed Talking Mats resource helps to open up conversations with young people about sex.
REACH is a unique team, one of a kind in Scotland, that provides intensive support for care experienced children and young people on the edge of care in Perth & Kinross. We are a multidisciplinary team bringing together professionals across health, education, social work and youth work. This allows us to provide prompt specialist care, while limiting the need for referrals to multiple agencies.
My colleague, Janie Scott, and I have worked for REACH since its inception, as Highly Specialist Speech and Language Therapists. Research shows that more than 60% of care experienced young people have some kind of speech, language and communication need (SLCN) and at REACH we work on the assumption that our young people may have an SLCN – until proven otherwise. This means that we routinely offer communication assessments and support to every single young person (and their parent/carers), in addition to keeping inclusive communication at the heart of everything we do. Adopting this approach ensures that none of our young people have to struggle with communication difficulties unsupported.
Working in a multidisciplinary team with a heavy social work contingent has been a very different experience for Janie and I. The team were open to our training and approaches and allowed us the freedom and autonomy to shape our own SLT service.
One of the first things we did at REACH was to introduce Talking Mats. We are both Talking Mats Licensed Trainers. All our REACH staff, as well as any other colleagues across the council and NHS who also work with our young people are Talking Mats trained.
Despite some initial scepticism around using pictures with teenagers, the resource has since proven to be incredibly useful and engaging for this particular client group. It has now become a staple resource that our staff will reach for regularly to facilitate conversations with our Young People and to help them express their views on complex issues.
Our young people can occasionally find themselves in conflict with the law and wrapped up in the complexities of the criminal justice system, as a result of their often disadvantaged backgrounds, and/or due to a range of ongoing challenges such as developmental trauma, social emotional and mental health difficulties, and/or Speech, Language and Communication Needs (SLCN). In addition to supporting REACH clients through their criminal justice journey, our team also specialise in harmful sexual behaviour assessments, for both internal and external clients.
The idea for a Talking Mats resource for harmful sexual behaviour initially came from one of our Senior Practitioner Social Workers, Amy MacKinnon, who suggested that Talking Mats might be a useful tool to support their harmful sexual behaviour assessments (AIM3). The assessment, which involves interviewing the young person about incredibly sensitive and personal issues, can be quite confronting for young people. We discussed the possibility of having visual resources which would not only cater to the SLCN of our clients, but that would also make the assessment feel less intimidating for the young people, encouraging more open and honest responses.
We often start by assessing a young person’s existing level of sexual knowledge and understanding, as how can young people possibly share their version of events if they do not understand the basic concepts of which they were being accused of?
This includes exploring their understanding of the language around sexual physiology and anatomy, in addition to the social and legal considerations of sexual behaviour. The introduction of this resource allowed us to explore existing knowledge much more effectively than we had previously, with a more logical progression of concepts ranging from the very concrete language for body parts, through to more abstract ideas such as consent. More careful consideration of the young person’s language level really helps to ensure that the Young Person’s responses are accurate. We recognised that our existing pictures/resources needed development and so I approached Talking Mats to ask if they would consider working with us to create an official Talking Mats resource using their own artwork and branding. I know from experience that their artist, Adam, always does a fantastic job creating simple images that are so easily understood while also being sensitive and inclusive.
We developed a small working group with a handful of REACH and Talking Mats staff who have focused on developing a new healthy relationships resource to open up these tricky conversations. We have now completed the pilot stage, and have a fantastic resource. Talking Mats did not disappoint and as expected, they worked wonders with the images!
One interesting development along the way was the group’s reflection that the resource had felt quite negative and that perhaps we should keep a more neutral stance when developing the concepts – leaving room for much more general (or even positive) discussions around sexual development too. This allowed us to expand the resource to include concepts relating to puberty and gender identity. We felt that this would make the resource more far-reaching and impactful, while still retaining the option to use the more niche resources for addressing harmful sexual behaviour, when required.
The feedback we have received has been overwhelmingly positive, with comments such as ‘It’s amazing’ and ‘We’ve been sitting waiting for a resource like this.’ Those trialling the resource for us unanimously felt that the resource helped them to discuss the topic with their clients, helping to ‘open up’ discussions that would otherwise be more challenging to initiate. We have also received a lot of positive feedback on the clarity of the concepts and images; the consensus being that the visuals are easy to understand and unambiguous. This is fantastic feedback given the complex and abstract concepts we were tackling with this resource!
We are looking forward to sharing more information about the project and resource in an Advanced Webinar for practitioners who have already completed Talking Mats Foundation Training, in September 2024.
Look out for the second part of Julia’s blog next week, to read one of the powerful examples of the positive impact this resource has already had.
Inspired to think about Talking Mats Foundation Training? Find out about all the options we have available here.
 Online training login
Online training login 



