The role of Talking Mats in supporting people to make decisions in a capacity context.
Context
At the heart of the different capacity legislation that covers England, Wales, Ireland and Scotland is a requirement to ensure that all practicable steps are taken to support the communication of an individual. Talking Mats is well suited to do this as, it supports people to understand, process and weigh up information and then helps them express their views.
Talking Mats has a research base that provides evidence that using this visual framework improves the quality and quantity of information people can give. This has been shown for people with learning disability, dementia and aphasia.
Capacity; enabling supported decision-making.
The Resource.
This resource has been developed with several teams working in different parts of UK. Capacity is decision specific and must be tailored to fit the requirements of the decision. In developing this resource we have focused on the most common decisions people face; what you do in your free time, where you live, your safety, and your support plan. This resource will not cover all capacity decisions but will be a helpful starting point to support you and your clients.
Why use Talking Mats to support decision making ?

- Decisions are broken down into manageable chunks that reduce cognitive load
- The use of visuals reduces the pressure on spoken language and assists the expression of views.
- It allows people time to reflect on their decisions and change their min
- It demonstrates areas that require more information and knowledge to help make a decision
The Advanced Online Course
This course has been jointly developed by practitioners from social work, occupational therapy and speech and language therapy. Course attendees will;

- Think about and extend their practice within the provisions of the Capacity Act relevant to them
- Think about how decisions are made and what affects the way they are made
- Learn how to extend the resource to cover specific decisions that are not covered
- Explore and reflect on their own use of Talking Mats in this context
- Share their experience and learn from others
Learning will be through short talks, interactive activities, case examples and small group discussion. There will be a mid- session screen break.
To join this Advanced Online Course you need to;
- Have completed the Talking Mats Foundation Training
- Attend with a system that allows you to join in the Teams chat during the session and go into small breakout rooms
- Book onto our Advanced Course via the website shop before the 7th of April
The cost is £95 and this covers the resource and the online session. Places are limited to make sure to book on soon. Resources will be posted out the week before training. Bookings close on the 7th of April.
Not yet Foundation Trained?
Talking Mats don’t do Pink Friday, Black Friday or Cyber Monday but we can tell you about our January Sale.
Starting on the 1st of January 2025 and running until the 31st of January 2025 we are offering;
- 30% discount on our Health and Well Being Bundle
- 30% discount on our Social Care Resource *
- 50% discount on our Eating and Drinking Resource *
*available if Foundation Trained
These are popular resources and over the next couple of weeks I will signpost you to some of our top blogs that showcase how they can be used.
This week:
Health and Well Being Resource Bundle

This comprehensive resource can support conversations around general health, a person’s environment, ability to look after themselves and their communication across different areas. Find out more about it’s development and use.
Read about the development and background to the resource and its use with Duncan who had had a stroke.
Kate was a woman with severe communication difficulties following a stroke. This blog describes how using the 4 communication topics Kate and her therapist were able to identify specific challenges that could be worked on to help her overcome her difficulties.
The Health and Well Being Resource complete with bag and mat will be reduced by 30% from the 1st of January and will be available to buy in the website shop from that date.
We are pleased to share a new blog from Talking Mat Associate, Jess Lane, as part of a 2-part series on the use of Talking Mats within Child and Adolescent Mental Health Services (CAMHS).
In Part 1, Jess described how Talking Mats can provide children with a safe space to explore topics that they might otherwise feel unable to communicate about, in a way that is highly supportive, sensitive and impactful. Check it out here:
In Part 2, Jess reflects on the use of Talking Mats by all members of the multidisciplinary team. We also hear from Nikki Low, Specialist Occupational Therapist, who reflects on her use of Talking Mats in the acute mental health setting.
Later in the blog, Jess explores how Talking Mats can be used as part of a post-diagnostic package of support for autistic children to support more focussed, strengths-based conversations, in line with the core principles of neurodiversity affirming practice.
A Multidisciplinary Approach
Welcome back to my 2-part series on the use of Talking Mats within CAMHS. In Part 1, I described how the implementation of Talking Mats by all members of the multidisciplinary team has transformed the way children are supported in the acute mental health setting. I have since reflected with clinicians from across Speech and Language Therapy, Nursing, Psychiatry, Dietetics, Occupational Therapy, Physiotherapy and Psychology on how Talking Mats continue to be used on CIPU to facilitate the direct and meaningful involvement of children in care planning, and to facilitate equity of access to therapeutic intervention.
Nikki Low reflects on using Talking Mats in her role as a Specialist Occupational Therapist:
“I am a Specialist Occupational Therapist working in a Psychiatric Inpatient Unit with children under 12, many of whom, in addition to their mental illness, have an intellectual disability, are neurodivergent and/or have experienced complex trauma. This can make meaningful interactions about thoughts and feelings challenging or even impossible, particularly when discussing sensitive topics.
We strive to provide a client centred approach to care and treatment for our young patients but this can be difficult when they are unable to express themselves. Talking Mats has revolutionised our approach with these children. It has proven to be a powerful tool, transforming communication experiences for individuals of all abilities. I have used Talking Mats to engage patients in assessments and to formulate their treatment goals. Its user-friendly design, customisable features and positive impact make it an invaluable resource in the care and treatment of our vulnerable young patients.
As a unit, we have rolled out training to all core staff in order that we can incorporate Talking Mats into our practice. By doing this, we have been able to facilitate more inclusive and person-centred interactions, ultimately fostering a more supportive and empowering environment for all involved.”
Implementing Talking Mats across a whole staff team has increased the capacity and capability of clinicians to routinely involve children in decisions pertaining to their care. It has also contributed to a culture whereby Talking Mats are considered at each stage of a child’s admission, to support assessments of capacity and mental state, medication reviews, engagement with advocacy services and participation in all multidisciplinary team meetings and case conferences.
Post-Diagnostic Support
Most recently, I have used Talking Mats as part of a post-diagnostic package of support for autistic children, to support more focussed, strengths-based conversations around what it means to be autistic. This has involved developing a symbol set based on SIGN guidelines and associated resources, to support children who have recently been diagnosed as autistic, to engage in a conversation about what would be helpful for them to know.
When presented with a Top Scale of Helpful, Not Sure, Not Helpful, children were able to share their opinion on a range of options, including (but not limited to): facts and figures, autistic famous people, links to other work, skills, strategies and resources. An example is provided below. From this, I was able to create a personalised information pack for each child, based on what they would (and would not) find helpful to know about autism.

Most children shared that it would be helpful to find out about autistic famous people. This provided the foundation for a follow-up conversation about identity. Some children shared that they would find it helpful to find out about incidence and prevalence figures. Others did not. This was reflected in their information packs. For children who shared that they would like to understand how being autistic might impact, or otherwise feed into, therapeutic work for anxiety, I worked with colleagues from across Psychology and Nursing to ensure this was accurately reflected in their information packs.
Using a Talking Mat to scaffold conversations about what it means to be autistic has been well received by other clinicians involved in providing post-diagnostic support. By providing children with an opportunity to identify exactly what they would like to know about autism, clinicians have been able prioritise areas of support and signpost to the most relevant resources. This speaks to legislation that calls for the greater involvement of patients in decision making, in line with the mantra: no decision about me, without me.
Anecdotally, I have found that using Talking Mats as part of a post-diagnostic package of support has made a significant contribution to the development of a more streamlined, relevant and person-centred approach to sharing information. Using Talking Mats in this way has provided children with a dedicated space to voice their opinion on a topic that they might not have previously inputted into, that has been actively listened to and directly acted upon.
It is hoped that in sharing how Talking Mats can be used as part of a post-diagnostic package of support, this blog might encourage others to consider how they might achieve similarly positive outcomes for children with other diagnoses. If you have used Talking Mats as part of a post-diagnostic package of support for children or adults, I would love to hear from you! Please do get in touch at info@talkingmats.com.
Do you work with people with intellectual disabilities and / or autism?
Researchers at the University of Hertfordshire have been working with Talking Mats to develop a range of symbols to help people with intellectual disabilities and/or autism to communicate symptoms of long Covid. It is hoped that these symbols will help facilitate conversations and improve accessibility to long Covid service pathways and improve health outcomes.
There are three topics that have been developed:
- Symptoms – This Topic uses a suggested Top Scale of I have / I sometimes have / I don’t have. Options in this topic include heart going fast , dizziness , brain fog.
- Mood – This Topic uses a suggested Top Scale of This is me / This is sometimes me / This not me. Options in this topic include frustrated, not interested, confident
- Getting Help – This Topic supports you to discuss how supported the individual feels and where their key supports are coming from. A suggested Top Scale is Going well / Unsure / Not going well. Options in this Topic include GP, online/phone support, specialist team.
This Talking Mats resource was developed in partnership with a group of people with intellectual disabilities and people with autism alongside a range of health professionals. People who had lived experience of long Covid were also involved in the group.
Participate and use the resource
We would like to hear from a wider cohort of practitioners working with people who have learning disabilities. For example, nurses, speech and language therapists and occupational therapists. We want to know if there is a need for this long Covid Talking Mats resource. This resource can also be used where long Covid has not been formally diagnosed but you want to listen to the person with a learning disability and hear about their experience of their long-term health condition.
If you would like to participate, and meet the following criteria, we would love to hear from you.
Criteria:
1. Have completed Talking Mats Foundation Training course.
2. Work in a setting supporting people with intellectual disabilities and/or autism.
If you would like to get involved, please complete the following survey by the end of April 2024.
Click here for the Long Covid Survey
Please note that should you consent to be involved in this project, your information will be shared with the University of Hertfordshire.
The team will be looking for feedback by the end of July 2024 and you will be asked to fill in a short survey for each Talking Mat that you complete . This survey will be sent to you alongside the long Covid resource.
If you have any questions about this, please do not hesitate to contact info@talkingmats.com
Our thanks for this guest blog go to Meredith Smith, Paediatric Physiotherapist and Lecturer in Physiotherapy in the School of Allied Health Science and Practice at the University of Adelaide. In this blog, Meredith talks about the development of a Talking Mats resource to facilitate self-reporting in pain assessments for children and young people with cerebral palsy.
Our research team has been working on modifying pain assessment tools so they are more appropriate, relevant and accessible to children and young people with cerebral palsy (CP). People with CP have varying functional, communication and cognitive abilities, which makes existing assessment tools (often pen and paper questionnaires) difficult to use across the spectrum of ability. As a result, children and young people with CP often don’t have the opportunity to self-report how pain is impacting their function.
We are based in Australia and our team is made up of physiotherapists, an occupational therapist, a medical practitioner, researchers and people with lived experience of CP. One of the first things we did as part of this project was to ask people with lived experience of CP and clinicians what we could do to make two specific pain assessment tools more accessible and relevant to people with CP and different abilities. One of the clinicians (a speech pathologist), suggested we consider a Talking Mat alternative for each of the assessment tools. These two assessments focused on two concepts – 1) how pain interferes with function and 2) pain-related fear. We were keen to focus on these assessments as this would help us to not only open up a conversation about pain with children and young people with CP, but would also provide us with a way of identifying children who might benefit from particular pain interventions, and allow us to monitor the effectiveness of these interventions.
Prior to this suggestion I had heard of Talking Mats but never used it. Our research team underwent Talking Mats foundation training which was excellent, and we were all really impressed with the concept and its application in varying contexts. We had initially thought that we might need a Talking Mat to get feedback from children on the assessment tools, but we all agreed that converting the pain assessment itself into a Talking Mat would make the most sense for now.
Working with the Talking Mats team was a fantastic experience. We all really appreciated the expertise of the consultants in considering how we worded some of the assessment tool items. The symbols created were also excellent, and when we tested them with children and young people with CP they were simple and easy to understand.
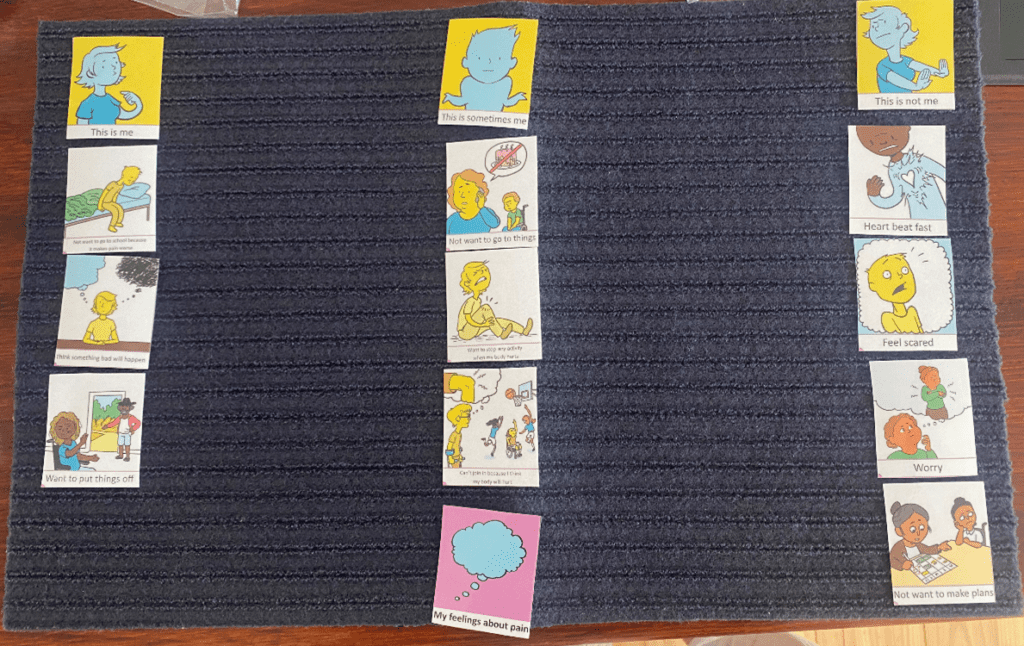
Here is an example of a Talking Mat discussing pain interference with function. The lead in phrase is ‘how much does pain get in the way of……’. This Talking Mat was easily understood by most children with CP, even those with moderate cognitive impairment and complex communication needs.

The second Talking Mat looked at pain related fear, with the lead in phrase ‘pain makes me……’. This was a more challenging and abstract concept, but was much easier to explore using the mat than on a standard pen and paper questionnaire. The Talking Mat versions can be interpreted as a 5-point response scale (the three response options and then two in-between sections), allowing us to still total an overall score for the assessment.
The feedback from children, young people and their families has been very positive. Families of children with cognitive impairment or complex communication needs have shared with us that previously it was assumed that their child could not self-report pain, and often they were asked to proxy-report on their behalf. Parents have told us how difficult it is to proxy-report on personal concepts such as pain-related fear, and that they couldn’t possibly know for certain how pain was making their child feel.
We are in the process of continuing to test the Talking Mats resource and look forward to making the it more widely available in the future.
Keep an eye on our website for more information about the Pain Assessment Resource as this project progresses.
If you are interested in completing Talking Mats Foundation Training, you can find out more here.
Talking about sensitive issues can be challenging at times. We are so excited to publish this guest blog from Julia Pollock, Highly Specialist Speech and Language Therapist (SLT) from the REACH team in Perth, Scotland, explaining how a newly developed Talking Mats resource helps to open up conversations with young people about sex.
REACH is a unique team, one of a kind in Scotland, that provides intensive support for care experienced children and young people on the edge of care in Perth & Kinross. We are a multidisciplinary team bringing together professionals across health, education, social work and youth work. This allows us to provide prompt specialist care, while limiting the need for referrals to multiple agencies.
My colleague, Janie Scott, and I have worked for REACH since its inception, as Highly Specialist Speech and Language Therapists. Research shows that more than 60% of care experienced young people have some kind of speech, language and communication need (SLCN) and at REACH we work on the assumption that our young people may have an SLCN – until proven otherwise. This means that we routinely offer communication assessments and support to every single young person (and their parent/carers), in addition to keeping inclusive communication at the heart of everything we do. Adopting this approach ensures that none of our young people have to struggle with communication difficulties unsupported.
Working in a multidisciplinary team with a heavy social work contingent has been a very different experience for Janie and I. The team were open to our training and approaches and allowed us the freedom and autonomy to shape our own SLT service.
One of the first things we did at REACH was to introduce Talking Mats. We are both Talking Mats Licensed Trainers. All our REACH staff, as well as any other colleagues across the council and NHS who also work with our young people are Talking Mats trained.
Despite some initial scepticism around using pictures with teenagers, the resource has since proven to be incredibly useful and engaging for this particular client group. It has now become a staple resource that our staff will reach for regularly to facilitate conversations with our Young People and to help them express their views on complex issues.
Our young people can occasionally find themselves in conflict with the law and wrapped up in the complexities of the criminal justice system, as a result of their often disadvantaged backgrounds, and/or due to a range of ongoing challenges such as developmental trauma, social emotional and mental health difficulties, and/or Speech, Language and Communication Needs (SLCN). In addition to supporting REACH clients through their criminal justice journey, our team also specialise in harmful sexual behaviour assessments, for both internal and external clients.
The idea for a Talking Mats resource for harmful sexual behaviour initially came from one of our Senior Practitioner Social Workers, Amy MacKinnon, who suggested that Talking Mats might be a useful tool to support their harmful sexual behaviour assessments (AIM3). The assessment, which involves interviewing the young person about incredibly sensitive and personal issues, can be quite confronting for young people. We discussed the possibility of having visual resources which would not only cater to the SLCN of our clients, but that would also make the assessment feel less intimidating for the young people, encouraging more open and honest responses.
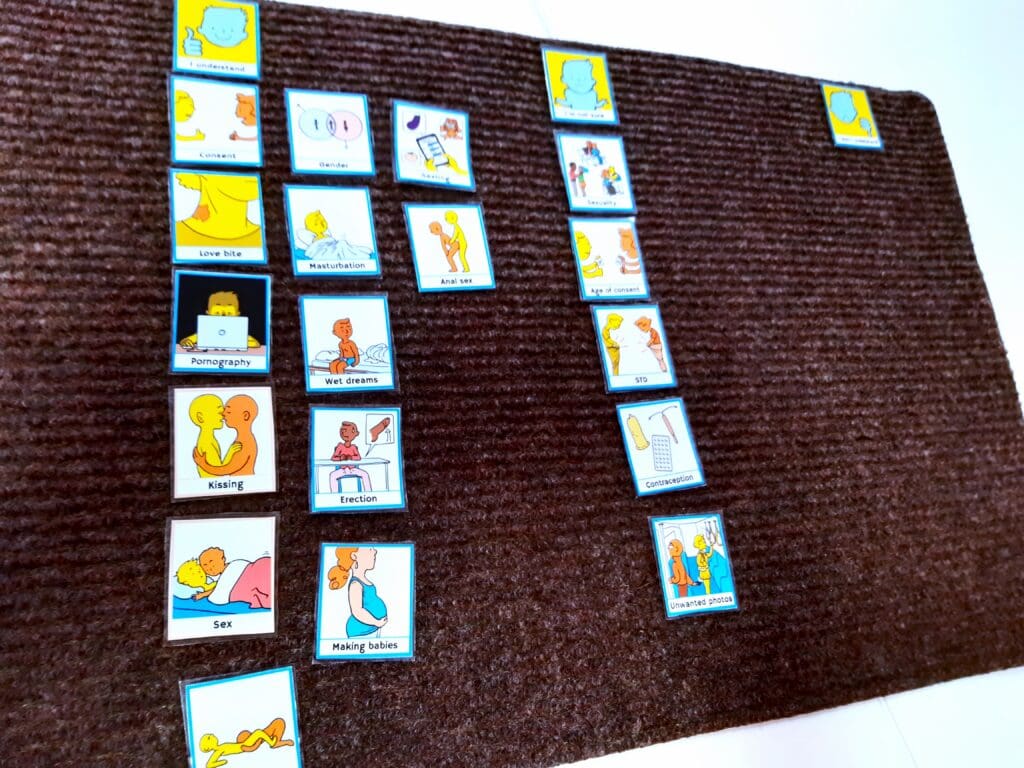
We often start by assessing a young person’s existing level of sexual knowledge and understanding, as how can young people possibly share their version of events if they do not understand the basic concepts of which they were being accused of?
This includes exploring their understanding of the language around sexual physiology and anatomy, in addition to the social and legal considerations of sexual behaviour. The introduction of this resource allowed us to explore existing knowledge much more effectively than we had previously, with a more logical progression of concepts ranging from the very concrete language for body parts, through to more abstract ideas such as consent. More careful consideration of the young person’s language level really helps to ensure that the Young Person’s responses are accurate. We recognised that our existing pictures/resources needed development and so I approached Talking Mats to ask if they would consider working with us to create an official Talking Mats resource using their own artwork and branding. I know from experience that their artist, Adam, always does a fantastic job creating simple images that are so easily understood while also being sensitive and inclusive.
We developed a small working group with a handful of REACH and Talking Mats staff who have focused on developing a new healthy relationships resource to open up these tricky conversations. We have now completed the pilot stage, and have a fantastic resource. Talking Mats did not disappoint and as expected, they worked wonders with the images!
One interesting development along the way was the group’s reflection that the resource had felt quite negative and that perhaps we should keep a more neutral stance when developing the concepts – leaving room for much more general (or even positive) discussions around sexual development too. This allowed us to expand the resource to include concepts relating to puberty and gender identity. We felt that this would make the resource more far-reaching and impactful, while still retaining the option to use the more niche resources for addressing harmful sexual behaviour, when required.
The feedback we have received has been overwhelmingly positive, with comments such as ‘It’s amazing’ and ‘We’ve been sitting waiting for a resource like this.’ Those trialling the resource for us unanimously felt that the resource helped them to discuss the topic with their clients, helping to ‘open up’ discussions that would otherwise be more challenging to initiate. We have also received a lot of positive feedback on the clarity of the concepts and images; the consensus being that the visuals are easy to understand and unambiguous. This is fantastic feedback given the complex and abstract concepts we were tackling with this resource!
We will be holding an Advanced Webinar for practitioners who have already completed Talking Mats Foundation Training, in February 2025.
Look out for the second part of Julia’s blog next week, to read one of the powerful examples of the positive impact this resource has already had.
Inspired to think about Talking Mats Foundation Training? Find out about all the options we have available here.
Many thanks to Karen Mellon, NHS Fife Lead Podiatrist for Learning Disabilities and Care Homes, for this guest blog describing our exciting Fife Health Charity funded project, aimed at supporting patients with a learning disability (LD), or dementia, to be more involved in decisions around their care.
I was initially introduced to Talking Mats by my Learning Disability SLT colleagues who were using the resource to support patient engagement. I could see the real benefits of how it could support our interactions with patients with a LD or dementia and empower people to be more involved with decisions around their care. Our SLT colleagues had undertaken the Talking Mats Train the Trainer program and were then able to train our podiatrists in using the resource. Having used the existing resources we found that we weren’t able to discuss/explore people’s views deeply enough, for example, when they developed a foot ulceration, or were at risk of ulceration. This was the spark that ignited the idea to look at developing a specific foot care resource to enable these conversations.
The aim was to promote patient engagement in their care – both in preventative care and when specialised input is required. By creating the resource we aimed to explore what really mattered to the person and what for them were acceptable goals and outcomes. By developing a specific Talking Mats resource we were able to explore treatments options and impact of conditions and actively engage the person in expressing their views thus creating a person centred care plan. Evidence shows us when people are involved in decision making they are more satisfied with their care, which in turns improves their quality of life.
Having consulted with Talking Mats we jointly created an initial resource which we piloted within NHS Fife over a 6 week period. People living within care homes and people with a learning disability were the target audience for the pilot. Using the resource, we were able to understand more about the impact that foot ulceration was having on patients, and patient’s views on treatment options.
One example of this positive impact involves a 60 year old patient with learning disabilities and dementia. She lives independently with one hour support each day to assist with personal care. She has been known to podiatry for some time due to repeated ulceration. Specialist footwear has been supplied and regular input is in place to reduce the risk of re-occurrence, however at times the foot does break down.
In May the patient experienced a break down on her foot. She is a very pleasant lady who always comes across as if nothing bothers her and everything is fine; she doesn’t like to “cause a fuss”. It was felt the use of a Talking Mat might give us greater insight into the impact the wound was having.
As a result of completing the Talking Mat we were able to discover the patient was in fact experiencing difficulties with the type of dressing and was experiencing pain. We were able to address this and change the dressing type to an adhesive dressing, which took up less room in her shoe, and started her on Paracetamol 4 times a day to address her pain. Follow up discussions reveal the patient was much more satisfied with the dressing, it was more comfortable and easier to keep dry when showering. She also reported to be experiencing much less pain.
As a result of the mat, we were able to identify concerns she had, but didn’t want to share as she didn’t want to be a burden. We were able to address this and create a plan which was acceptable to the patient and improved her wellbeing.
I hope this resource will go on to benefit other professionals and carers working with people who may be impacted by their foot health. By using this resource, we can help our patients explore their views and wishes, therefore enabling co-production in care. The resource promotes preventative care as well as specialist intervention. Going forward there are many other areas of foot health that could potentially be explored in developing further resources – such as paediatrics, nail surgery, musculoskeletal.
Book your place on the Talking Mats and foot care training course on 24th January 2024 / 21st February 2024 being run jointly between ourselves and Karen Mellon . The price includes the resource .
To find out more about the work and projects supported by the Fife Health Charity follow their Social Media accounts at:
Facebook – @fifehealthcharity
Twitter – @FifeHealth
 Online training login
Online training login 



