Get involved in choosing a Communication Access UK Symbol , and set the standards to go with it!
In early 2017 Communication Matters[1] found out that –
- People with communication difficulties don’t always get the support they need in the community.
- People would like a Communication Access symbol in the UK. Businesses already use some symbols e.g
A small group of people were asked to choose a symbol to represent Communication Access. 2 ideas were very popular. For an organisation to display this communication symbol it will mean the staff have been trained to support communication and that the business meets certain standards
Communication Matters now want to hear from more people, with and without communication difficulties.
To have your say about 1) the symbol and 2) the standards to support communication follow this link. http://www.talkingmats.com/wp-content/uploads/2017/12/Communication-Access-UK-Symbols-and-Standards.pdf You will find the symbol choice and a Talking Mat to decide what is important to include in the Communication Access Standards. Send your responses to Communication Matters
Email : admin@communicationmatters.org.uk
Or post : Communication Matters, 3rd Floor, University House, University of Leeds, LEEDS, LS2 9DF
[1] http://www.communicationmatters.org.uk/
Huge thanks to all the practitioners who have sent us guest blogs. We selected our 10 favourite guest blogs…in no particular order!
- Talking Mats to support children who stammer Kirsten Taylor, Speech and Language Therapist tells a moving story about how finding out what was upsetting a boy with a stammer helped to implement change.
- Hearing the voice of the child Emma Atkiss, Senior Educational Psychologist, shares her findings from the Wigan Pathfinder project reporting that using a Talking Mat helps to meet the 5 criteria of Shier’s model of participation.
- Talking Mats for capacity assessments in people with ASD/LD Ruth Spilman, Senior SLT from The Cambian Group, shares practical tips on assessing capacity.
- Castle hill school supports pupil voice Jenna McCammon, SLT and Rebecca Highton, SLT Assistant, tell 3 inspiring stories using TMs in: selective mutism; safeguarding and motivational interviewing.
- Supporting Looked After Children to have their say Karen Wilson, Principal Teacher for children with additional support needs in a mainstream secondary school shares her experience of using TMs to give young people a stronger voice in making decisions affecting them.
- Hearing the voices of Looked After Children Rachel Clemow, Head Teacher and Donna Wood, Education Support Worker, report that Talking Mats has enabled children to express their thoughts and views in a safe, neutral environment.
- Talking Mats and Mental Health Carla Innes, Clinical Psychologist for learning disability from Healthy Young minds Stockport talks about the impact of TM training on the whole team.
- Mummy I don’t want to go to nursery today read about how using a Talking Mat might shed some light on why a 4 year old was upset at the thought of going to nursery.
- How do you feel about starting school? The story of 4 year old twins and their thoughts about starting school.
- Sibling Attitudes Prof Juan Bornman from Pretoria in South Africa publishes a report on a study carried out with 27 typically developing children who have a younger sibling with a severe speech and language disability.
If you have been inspired and are not yet trained to use Talking Mats – come along to one of our training courses.
This is the second blog about Lois and Nicki’s amazing visit to Australasia – this time theirTalking Mats trip to New Zealand.
The view flying into New Zealand was dramatic. We looked down on a beautiful range of snow topped mountains glistening in the clear blue sky as our plane flew towards Christchurch. Our first stop was the South island for a foundation training organised by Talk Link. Our second foundation training was in Auckland in the North Island. At both places we had a fantastic group of interested practitioners who really engaged with how Talking Mats could be used and began thinking creatively about how they would apply in their work place .This included:
• Involving thinkers in decisions about the their alternative and augmentative communication and getting feedback on what works for them
• Exploring its value for young people in the youth justice system to support them to express their views and be a tool for increasing engagement
• Exploring how Talking Mats could be adapted to make them more accessible and culturally accepted to the Maori community
• Involving children in their education planning
We were really pleased that Talk Link also sent 3 staff to the accredited training course in Australia. This means that there will be increased access to Talking Mats Foundation training in New Zealand for the future. Our experience is that accredited trainers provide leadership that helps organisations embed Talking Mats into practice. Thanks to Ann Smaill for all her organising and support for both our Foundation and Accredited courses.
And our leisure times were special too. We had a trip on the Christchurch Gondola to see the stunning Banks peninsula; we experienced the hope and resilience of Christchurch following the earthquakes in 2010 and 2011. In Auckland we saw a thought provoking Maori exhibition and last but not least we loved our weekend of rest and relaxation on the very special island of Waiheke. The locals thought us mad to swim in the sea their autumn but we loved it!
More information
Click for more information if you want to find out about
Many thanks to Greg Cigan for this great blog about his study that explored how children and young people with an intellectual disability feel about undergoing clinical procedures.
A clinical procedure is any activity performed by a healthcare practitioner to diagnose, monitor and/or treat an illness such as blood pressure testing, x-rays and other scans (Cigan et al., 2016). While some procedures cause no pain or only mild discomfort when completed, others can be prolonged and potentially painful (Coyne and Scott, 2014). Children and young people with an intellectual disability are more likely to develop physical illnesses including epilepsy and digestive disorders than the general population and can be frequently required to undergo healthcare procedures (Emerson et al., 2011; Short and Calder, 2013). Yet, there is currently little empirical research reporting how children and young people with an intellectual disability experience procedures (Peninsula Cerebra Research Unit, 2016). More research is required so that healthcare services can better understand the needs of children and young people with an intellectual disability (Oulton et al., 2016). As part of my doctoral studies at Edge Hill University, I am conducting a study that explores how children and young people with an intellectual disability experience having a clinical procedure.
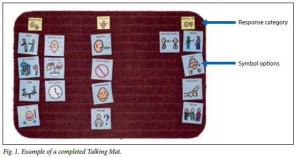
From the outset of the study, I felt it was important to obtain data directly from children and young people rather than relying on parents and carers to speak on their behalf. I was keen to adopt methods during interviews that would enable as many children and young people as possible to take part, including those who find verbal communication challenging. After researching different methods, I chose to utilise Talking Mats as the innovative design of the tool offered children and young people the option to express their views entirely non-verbally should they wish to by arranging symbol cards. To date, I have interviewed 11 children and young people about their experiences of undergoing procedures. Each participant was between 7-15 years of age at the time of the interview and had a mild to moderate intellectual disability.
Prior to an interview beginning, I spent time describing and showing each child/young person a Talking Mat and asked whether they would like to use the tool during their interview. Out of the 11 children and young people I have interviewed, three used a Talking Mat. Those that chose not to use the tool were older children who were confident having a verbal conversation with me or those who had a visual disability and could not see the symbols. In all cases, the decision of the child/young person in relation to using the Talking Mats was respected.
The three children who used the Talking Mats were able to express their views non-verbally and also seemed to convey more information than some of those who chose not to use the tool. Viewing the symbol cards within a Talking Mat appeared to help children and young people break down information into smaller chunks which then made it easier for them to process and discuss. Indeed, using a Talking Mat led all three children to discuss information that was new to their parents who sat in while s/he was being interviewed. An example of a completed Talking Mat is shown below which was created by an 11-year-old boy during his interview. The boy clearly expressed that he did not enjoy his experience of having a clinical procedure.
Within my study, I feel using Talking Mats has helped to augment the verbal communication of some of the children and young people which in turn enabled them to take part in interviews and share their views and experiences of procedures. Talking Mats are a valuable tool for researchers working within the field of intellectual disabilities. If used more widely, Talking Mats has the potential to enable more children and young people with intellectual disabilities to have the opportunity to be involved and express their views within healthcare research.
Reference List
CIGAN, G., BRAY, L., JACK, B. A. and KAEHNE, A., 2016. “It Was Kind of Scary”: The Experiences of Children and Young People with an Intellectual Disability of Undergoing Clinical Procedures in Healthcare Settings. Poster Presented at the 16th Seattle Club Conference (Awarded Best Poster Prize), 12-13 December. Glasgow: Glasgow Caledonian University.
COYNE, I. and SCOTT, P., 2014. Alternatives to Restraining Children for Clinical Procedures. Nursing Children and Young People, 26(2), pp. 22-27.
EMERSON, E., BAINES, S., ALLERTON, L. and WELCH, V., 2011. Health Inequalities and People with Learning Disabilities in the UK: 2011. Lancaster: Improving Health and Lives: Learning Disabilities Observatory.
PENINSULA CEREBRA RESEARCH UNIT, 2016. What’s the Evidence? Reducing Distress & Improving Cooperation with Invasive Medical Procedures for Children with Neurodisability. Exeter: University of Exeter.
SHORT, J. A. and CALDER, A., 2013. Anaesthesia for Children with Special Needs, Including Autistic Spectrum Disorder. Continuing Education in Anaesthesia, Critical Care & Pain, 13(4), pp. 107-112.
If you would like more information about Greg’s work you can contact him at Cigang@edgehill.ac.uk
Exploring sibling attitudes towards participation when the younger sibling has a severe speech and language disability
We were delighted to receive this publication from a friend and colleague, Prof Juan Bornman from Pretoria in South Africa. It reports on a study carried out with 27 typically developing children who have a younger sibling with a severe speech and language disability. Juan and her colleagues used Talking Mats to carried out an adapted structured interview to find out the views of these children on four everyday life situations identified by the WHO-ICF-CY (World Health Organisation’s International Classification of Functioning, Disability and Health, Children and Youth Version).
The four topics were:
Communication
Domestic life
Interpersonal interaction and relationships
Major life areas.
The findings showed that the children were ‘most positive towards participation in play activities with their sibling with a disability. They were also positive towards participation in household tasks. They were less positive towards communication participation and least positive about participation in interpersonal relationships’.
The following example is taken from Juan’s publication.
The article’s reference is:
Exploring sibling attitudes towards participation when the younger sibling has a severe speech and language disability. M Hansen, M Harty, J Bornman South African Journal of Child Health 2016 Vol. 10 No. 1
To read the full publication with details of the methods used and the results click here sibling-attitudes-2016
Delighted to introduce you to ‘The Communication Game’ : a board game for staff to improve their communication skills.
How we listen, talk and engage with people is fundamental to the quality and effectiveness of health and social care services. Although communication underpins everything we do in a work context, it can be a difficult topic for staff to talk easily about. Add to that the possibility of service users having an additional communication support need, through reasons like stroke, learning disability or dementia, then there is much potential for things to go awry and unfortunately, they often do. ‘Poor communication’ is cited as the most common cause of frustration in complaints about services.
The Communication Game was developed by Focus Games, NHS Education for Scotland (NES) and Talking Mats. It is a learning tool to help staff working in the health & social care sector increase their knowledge and skills around communication. The Communication Game is fun and easy to play. It can be played with or without a facilitator, and allows staff groups to have discussions and reflect on their communication skills. It allows them the chance to learn from each other. It will improve knowledge, but more importantly enable them to think about the small steps they can make to improve their interactions.
The project grew out of two previous projects funded by NES: Making Communication Even Better and Through a Different Door. In these projects, it was recognised that the experience of services for people with a communication support need is something of a lottery. For them, there was a considerable difference in the experience of interacting with a staff member who was empathetic and able adapt to their communication, to interacting with a member of staff who was struggling and unable to adapt their interaction. Training and understanding of inclusive communication practice is key. It has been a great privilege for Talking Mats to continue to support the work of the previous 2 projects and work with Focus Games Ltd to develop The Communication Game. Support during the development process from the Stroke Association Scotland, Capability Scotland, RCSLT, Scottish Care, Communication Forum, Queen Margaret University and NHS Ayrshire & Arran SLT Department have been invaluable, and we are very grateful; also to NHS Education for Scotland for their continued input and funding.
If you are working with staff in the health and social care sector, then this will be a great resource for you. You can get The Communication Game from the Focus Games online shop. It is guaranteed to promote laughter learning, and a touch of competitive team spirit. Most importantly, it will be a catalyst to help develop staff communication, making interactions better for people with communication support needs.
You can find out more about the game at www.communicationgame.co.uk
, and follow the game on Twitter on @Comm_Game.
Get your copy at www.focusgames.com.
We are very grateful to Anna Volkmer for sending us this blog, Lets Talk about Capacity…
She has just had an excellent book published – Dealing with Capacity and Other Legal Issues with Adults with Acquired Neurological Conditions http://www.jr-press.co.uk/dealing-capacity-legal-issues.html. In it she describes how AAC methods, including Talking Mats, can be used to support people in expressing their decisions.
Prior to 1959 people who were considered “non-compus mentis” were cared for under the “parens patriae” principle. Literally translated this meant that they were ‘parents of the country’ and decisions to protect them and their property were made by the Crown (the Lord Chancellor). These people were often described as “Chancery Lunatics”. In 1959 the “parens patriae” jurisdiction gave way to the Mental Health Act. This Act instructed that “the judge may, with respect to the property and affairs of a patient, do or secure the doing of all such things as appear necessary or expedient…for making provision for other persons or purposes for whom or which the patient might be expected to provide were he not mentally disordered” (section 102 (1)(c)). Unfortunately, this Act did not make adequate provision for non-financial decisions such as medical decisions. During this period it was case law that guided professionals in supporting their patients who lacked capacity in medical decision making. It was not until 2005 that the first Mental Capacity Act was given Royal Assent, accompanied by the Mental Capacity Act Code of Practice in 2007.
I returned to the UK from a 5-year stint working in Melbourne, Australia, just after the Mental Capacity Act had been published. Mental capacity was on the tip of everyone’s tongues and as the speech and language therapist working on a multi-disciplinary team I became an integral part of this process. Patients I was seeing, often people with primary progressive aphasia or other types of dementia, were asking about how to make future decisions. They and their families were keen to understand how the mental capacity act worked, how to prepare for the future and how to have their voices heard. On the other side of the coin I was working on an inpatient ward where staff were concerned about ensuring we were fully assessing the decision making capacity of people with cognitive and communication difficulties, often holding best interest discussion to plan for the future of these individuals. Many of these decisions related to dysphagia, but others related to accommodation and finances.
What concerned me was the lack of evidence available across the speech and language therapy arena in this area. There was little to none in terms of written research, let alone written advice or even examples of good practice tailored to speech and language therapy clinicians. As I asked around I found an enormous disparity in the services that speech and language therapy clinicians were providing across different trusts. I had previously written a book on dementia, and had included a chapter on assessments of decision-making. At this stage some of the only research related to communication and decision-making had come from Talking Mats. This had demonstrated that using the talking mats tools can support families and caregivers in conversations with their loved ones when discussing decisions to be made. They found that conversation enabled people in understanding, retaining and expressing themselves in decision-making discussions.
Following a particular stimulating discussion with the publishers at J&R press, they invited me to submit a book proposal on this topic. As I was developing this idea I found the topic of mental capacity was raised more and more often at study days and seminars I attended. At these study days I started linking in with more like minded speech and language therapists such as Mark Jayes, Hannah Luff and Claire Devereux. These were clinicians who all agreed on the diversity of our potential role in supporting our patients around mental capacity issues. These common interests enabled a collaboration. Our book is now published.
Through these connections I became aware of other work being done; Mark Jayes holds a NIHR doctoral fellowship award and is conducting research in the development of a communication and capacity assessment tool kit. Claire Devereux is the chair of the Southern Psychiatry of Old Age Clinical Excellence Network, together we have held a workshop with the clinical specialists where we developed a consensus document on role of the speech and language therapist in capacity assessment. This is to be published in Bulletin magazine later this year. Hannah Luff is a clinical lead speech and language therapist at South London and the Maudsley NHS Trust and is currently a member of the review panel looking at the NICE SCIE dementia guidelines.
The wonders and value of networking never ceases to delight, enthuse and inspire me! And you can purchase our book at the following website (there is currently a discount rate until 21st February):
http://www.jr-press.co.uk/dealing-capacity-legal-issues.html
You can follow me on my blog https://annavolkmersbigphdadventure.wordpress.com/ or on twitter @volkmer_anna
We are very grateful to Kristine Pedersen from Kommunikationscentret in Denmark for sharing the findings of 2 projects with us. The first project found Talking Mats was effective in supporting communication for people who have dementia when compared with both unstructured and structured conversations.
‘t is important to know how to give people with dementia the right support’
At Kommunikationscentret in Hillerød (Denmark), we have been using the Talking Mats framework since our first trainer was accredited at the Talking Mats Centre, University of Stirling in 2010. We have been using Talking Mats with both children and adults across a range of communication difficulties e.g. caused by Aphasia, Cerebral Palsy, Downs Syndrome, learning difficulties etc. Inspired by the important research project by Dr. Joan Murphy and others ‘Decision making with people with dementia’ (2010), our next step was to gain our own experience within the framework specifically aimed towards people with dementia.
As in the rest of the world, the number of people in Denmark with dementia is increasing. Symptoms of dementia vary from person to person but many of the symptoms are related to communication: Difficulties finding words, using familiar words repeatedly, losing track in conversation, difficulties in focusing and paying attention etc. The growing dependence of the person with dementia on a caregiver makes communication essential to express wishes and needs. Therefore, it makes sense to look at the consequences of the illness (dementia) within the perspective of communication and how family members and professionals around the person with dementia can support communication using AAC.
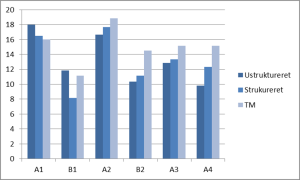
The purpose of the first project was to compare the communication in conversations about views on I) Daily activities and II) The importance of information, using three different communication methods. The methods were: 1) unstructured conversation 2) structured conversation 3) the Talking Mats framework. The project involved 6 participants having early to moderate stage dementia, all living in residential care homes.
Like the study ‘Decision making with people with dementia’ (2010), the report concludes that the Talking Mats method was associated with better communication for the majority of the participants. The Talking Mats framework was found especially helpful regarding the participant’s ability to understand subject and question of the conversation, the participant’s ability to reflect, and the participant’s ability to make themselves understood. The graph below shows that only one participant (A1) did not benefit from the visual method. She had poor eyesight, which strongly indicates that visual support compensates the difficulties that people with dementia have.
The report also concludes that the Talking Mats framework increases the interviewer’s ability to detect and compensate for some of the communication difficulties. Finally, it seemed that several of the participants have been able to learn how to use Talking Mats in the process.
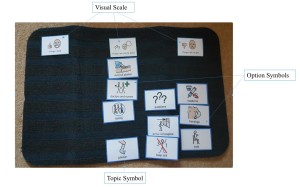
The photo underneath shows a Talking Mat conversation from the project. This Talking Mat gives an insight into how this person feels about what information is important to her, and what isn’t. It is in some way a difficult and abstract question, but most of the participants managed to both understand, reflect and answer the question when we used the Talking Mats framework.
Important information to this participant is information about new neighbours, the menu at the residential care home, economy etc. Less important is news about the Danish royal family, technology, getting older etc. Politics is definitely not important to her.
We are delighted that Nick Stewart, Director, Software and Products with Arum Systems, the IT Consultancy who have built the Digital Talking Mats has chosen TM as his favourite project for a case study.
Here is an extract from his case study describing the Challenge and Process of working with Talking Mats.
The Challenge
The challenge was taking the existing physical Talking Mats tool and building a digital application suitable for multiple platforms, while maintaining the core ethos of the tool. A significant amount of academic research went into creating the physical product and those principles had to be present in a digital version. The applications had to be extremely intuitive to use and enable better conversations for people with communication difficulties.
The aim was to create 3 digital versions; a browser based version for laptop users and a tablet version for iPad users and Android users. Each application would connect to a cloud server, allowing users to log in from any device, and the tablet versions would allow offline working through syncing with the cloud when a connection was available. There was a requirement to set up a multi-tiered subscription based user account system to match the intended charging model for the digital app.
Our Process
Arum’s approach was to totally immerse ourselves in the Talking Mats business to understand their goals, ethos and objectives. We took time to learn how the Talking Mats ecosystem worked and how they wanted to engage with their customers. By applying our 3D Methodology we were able to break down the deliverables into phases allowing the key building blocks to be delivered first. This also allowed the best use of budget and reduced the time to market the new product.
To read the full case study click here Arum Talking Mats Case Study
- This tool will be useful in helping some residents make decisions, informed choices and express their needs. It will take time for some residents to feel confident in using this tool.
- I’d like to use it with some residents to be able to adapt Talking Mats more to their understanding.
- I’d like to use this tool for resident’s reviews to find out what the residents likes/dislikes are.
- Talking Mats will be great for service evaluation.
- Talking Mats will be great for asking residents about things they want to do.
- Updating Care Plans regularly from outcomes of Talking Mats.
- It can be used to get to know people’s needs and wishes more.
- Share the findings with colleagues and joint services.
- Hopefully through its use I’ll learn to pass it onto others.
- A gardening set. Service evaluation and well-being assessing stress levels/anxiety/emotional state?
- I’d use it to promote choices of activities.
- Care Inspectorate forms. Finding out how people enjoy time at the service and how to improve on it.
Can you let us know how you use Talking Mats as part of your work?
 Online training login
Online training login