We are all continuing to live in challenging times due to the COVID-19 pandemic, and there are concerns about the impact on the mental health of people at all ages and stages of life. This is a good time to reflect on the wide variety of blogs that have signposted how useful Talking Mats can be in helping people to think, structure coherent responses, and express their views. If this is an area of interest to you then take a look at these blogs to find out more:
- Debbie Mole, Clinical Nurse Consultant in Mental Health and Intellectual Disability for DHM Mental Health Care in Melbourne, Australia shares a great example of the positive impact Talking Mats can have for people who have experienced trauma. https://www.talkingmats.com/talking-mats-and-trauma-work/
- Natalie Paris, CashBack 180 Project Lead shares some powerful examples of how Talking Mats has helped her to open up conversations with the young people she works with https://www.talkingmats.com/opening-up-conversations-with-young-people/
- Edith Barrowcliffe from The Action Group demonstrates how Talking Mats has allowed individuals with intellectual disabilities access talking therapies and counselling. https://www.talkingmats.com/counselling-communication-1/
- Edith expands on this work in her second blog, describing how she adapted this approach to use during remote support during lockdown. https://www.talkingmats.com/counselling-learning-in-lockdown/
- Jo Brackley, NHS Clinical Lead for SLT Secure Services (Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust) describes how Talking Mats helps people with mental health open up and have richer conversations, with increased novel information gained. https://www.talkingmats.com/covid19_securehospitalsetting/
- Susan Gowland, SLT at NHS Fife Forensic Learning Disability Service, describes how Talking Mats support patients to express what they think in forensic learning disability setting. https://www.talkingmats.com/forensic_ld_setting/
- Dr Carla Innes, Clinical Psychologist for Learning Disabilities at Stockport Healthy Young Minds (CAMHS) describes how Talking Mats helps the team to gain more insight to the children and young people they are working with, and how it has helped intervention focus on the child’s potential, and zone of proximal development. https://www.talkingmats.com/talking-mats-and-mental-health/. This work in Stockport is further expanded on in a presentation by Dr Rosie Noyce, Clinical Psychologist, given at the Talking Mats 21st Birthday Event in August 2019. https://www.talkingmats.com/wp-content/uploads/2019/08/Talking-Mats-and-Young-Peoples-Mental-Health.pdf
- Georgia Bowker-Brady, Advanced Specialist SLT (Berkshire Healthcare Foundation Trust) describes how using Talking Mats in dementia care and acute health patient inpatient services helps patients organise their thoughts and express what is going well for them, as well as what isn’t. https://www.talkingmats.com/acute-mental-health/
- Rachel Woolcomb, Talking Mats OT Associate, explains why Talking Mats supports thinking, and why it can be particularly useful in helping people to structure and express their thoughts. https://www.talkingmats.com/talking-mats-as-a-thinking-tool/
We would love someone to carry out some research in this field, so if this sparks a research or blog idea, please get in touch with us at info@talkingmats.com.
Many thanks to Natalie Paris, CashBack 180 Project Lead for our latest guest blog. Natalie shares some powerful examples of how Talking Mats has helped her to open up conversations with the young people she works with:
I joined Y2K Mayfield and Easthouses Youth 2000 Project in February 2018 as a sessional worker looking to gain practical experience in youth work, I then became Part Time Young Women’s worker at Y2K, which gave me experience in working with vulnerable young women in Midlothian across an age range of 11 to 24, some with mild to moderate learning difficulties. When I first heard about the 180 project, I knew it was something I really wanted to be involved with, as I have always been interested in Criminology and Youth Offending.
In September 2018 I became the full-time 180 Project Lead, and have helped to shape and develop our CashBack 180 Project. CashBack 180 is a referral-based service, focusing on early support and prevention for young people involved in or at risk of becoming involved in offending, anti-social and risky behaviours.
The Project:
We work with young people to make positive changes in order to work towards more positive futures. Young people accessing this service have the opportunity to take part in fun, participative and educational programmes of activities as well as 1:1 supports. The CashBack180 programme is delivered at Y2K, but we can also deliver programmes within High Schools.
CashBack 180 offers a menu of options and has adapted where necessary for our journey through the pandemic.
- 1:1 supports
- Groupwork programmes
- Community outreach support through detached youth work
Case Example 1:
A 12-year-old girl had been referred to me for violence, as she had attacked a girl in the playground, which was out of character for her. She was very uncomfortable in the 1 to 1 session, so I used a Talking Mat. This made the conversation flow more naturally.
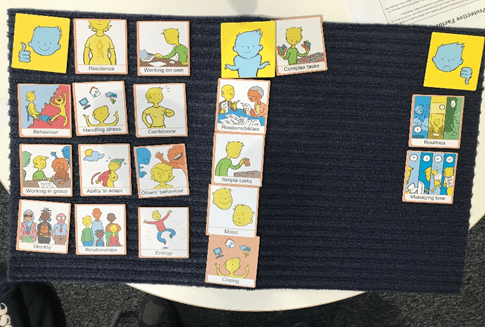
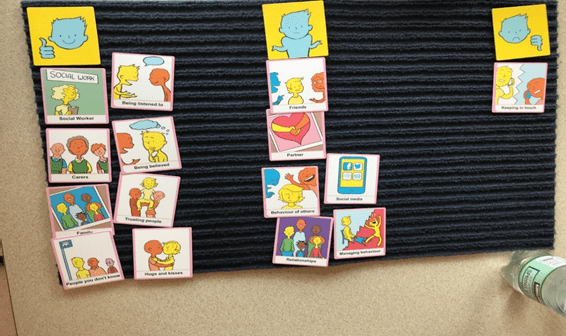
I used the Relationships topic, with the top scale ‘going well/okay/not going well’. This helped me get more information. I found out that most of the issues she was having were around peer relationships. For example, friends saying things that weren’t true, and not being believed by others in her friendship group. This allowed me to plan a session around what is healthy and unhealthy in friendships.

Case Example 2:
I was working with a 14-year-old care experienced boy, who had been referred to me for Anti-social behaviour, and because he was easily led. Once I got to know this boy a little better, I realised that he did not have much support within his family, apart from his older brother who he lives with now. I realised he was someone who had just learned to cope himself, and probably didn’t have many people to turn to when worried about things. I thought coping would be a good topic for a Talking Mat, as he always said things were fine, but I didn’t feel it was the full truth. I used the top scale ‘going well/okay/not going well’. This gave us the opportunity to discuss healthy and unhealthy coping mechanisms that he had and what he could do instead.
Case Example 3:
I was working with a 12-year-old care experienced boy, who had been referred to me due to his inappropriate sexualised language and reference to sexual experience. He has been out Mainstream school for 1 year, so had missed P7 sex education. I decided to start working on friendships and relationships over the first couple of weeks with him, to get an understanding of what he knew was acceptable in relationships. I used the Relationships Topic with the top scale ‘Going well/Okay/Not going well’. The Talking Mat helped me keep his attention for a little longer than usual, as he is a very chaotic young person and often gets up and walks about, or jumps on tables and pretends to be sleeping. It also showed me that he felt quite happy but was missing his friends from where he used to live. We are now looking at ways to address this.
Follow this link to Find out more about this project:
180 Service – Mayfield and Easthouses Youth 2000 Project
If you are feeling inspired and would like to know how you can access Talking Mats training, find out more here: https://www.talkingmats.com/training/
We are delighted to share this latest guest blog from Debbie Mole, Clinical Nurse Consultant in Mental Health and Intellectual Disability for DHM Mental Health Care in Melbourne, Australia. This is a great example of the positive impact Talking Mats can have for people who have experienced trauma.
Throughout my 35 year career I have always had a big interest in finding ways to help clients express themselves. My passion is around trauma and working in creative ways to help bring some closure and recovery for the person.
This desire grew when I met a woman who had multiple disabilities. She was blind, deaf, and non-verbal. She was sensitive to touch and had very few ways to express herself. She needed to be admitted to hospital as she was unwell, we had no way to explain to her what was happening. At the time I was working in a new specialised mental health and disability team. This humbling experience of working with her pathed a way for me to find ways to help people communicate and understand.
Working in mental health I am acutely aware of risks and that so many people who struggle to verbalise thoughts, feelings, and past issues. I was always concerned that because a person could not verbalise their thoughts, feelings, and intentions that so much information and potential risks were being missed.
I heard about Talking Mats training in Australia and booked myself on the course. This inspired me and has helped me support clients to find a voice and solutions to issues.
My client was a 30-year man with Down Syndrome, he also has ASD and over the last five years had lost his ability to speak. When I met him, he had poor eye contact and appeared to be locked into his world. It was evident he was also suffering from psychosis as he was responding to auditory and possibly visual hallucinations. He could use some sign language to communicate. He had chronic OCD and anxiety and sleep was a major issue.
I did a Talking Mat exercise and checked his understanding of “like”, “don’t like” and “not sure”. I did a simple exercise to start using the images for his family and carers. There was no real form and the cards appeared to become a collection of images that did not hold any clues.
I decided to use to the personal care cards, this was very different. Showering, bathing, and going to the toilet were placed in the negative area. There was also a change of behaviour and some vocalisation of words that made no sense. Talking to his team and mother, there was a restive quality to his behaviour – he wanted to avoid this area.
I did further assessments and his mom believed that in the past when he was young, he may have experienced some bullying, she also feared that he had suffered some form of abuse. Through the assessment it also transpired that my client was one of five children, all had a significant mental health issue. I organised a specialist to see him and he was diagnosed with Schizophrenia. He was treated with antipsychotic medication.
As the psychosis was being treated his team became aware that my client was starting to talk, it was not clear, but the content had a theme. Tragically themes, names and places started to be spoken about. When he spoke about these events his OCD behaviours of arranging his items on the floor became more chaotic. He spoke of trauma from other boys that took place in bathrooms.
I worked with the client and introduced some basic trauma work, simply allowing him to say what he wanted to and then helping him to realise that he was safe and that was the past. His team did the same. We offered choice about showering, bathing and looked at ways it could be fun or a nice activity to follow. The idea was to change his thinking around baths and showers and for him to realise he was safe and free from threat. We used the talking mats to build upon the things he liked.
I repeated the Talking Mats exercises three, six, nine and twelve months after treatment.
After the psychosis was treated, we became aware that the client looked sad and flat. There was a loss of interest in social activities and there was a lot of talk about the past. We assessed that he was depressed and that it was possible that his recall about the past was becoming clearer. He was commenced on an antidepressant and monitored intensely. We also needed to address the sleep issues. His OCD had led to his bed to being covered in items. We later realised that this helped reduce his anxiety when he was heightened.
My client has regained some speech, I believe he was locked in a world of trauma and psychosis. Now he mentions the names of some of the people who have hurt him. His team reassure him that he is safe, that was the past, and he is ok. He seeks physical attention when he distressed, and he is acknowledged and reassured. We cannot offer typical trauma therapy to him, but just helping him unlock his thoughts, knowing that what was happened was wrong and being heard is healing.
I have since developed my own set of cards, based on the Mental State Examination. I use these to expand on issues and focus on problem areas. These cards talk about perceptual issues, thought problems, beliefs and risks, all areas that are typically private and too often unexplored. The cards have images on them, so clients who struggle to verbalise can use the same system as the talking mats.
Talking Mats allowed me and his team to see things from a different angle. There were many hypotheses used to gain an understanding of his behaviour. This led to effective treatment and partial recovery.
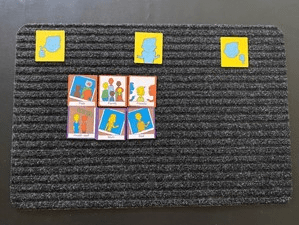
Picture 1 at the assessment stage, images of the clients family were made into an orderly collection with no clear indication of how he felt towards the images:
Picture 2 was also at assessment, showing a clear ability to like, not like and feel unsure about aspects of self care.
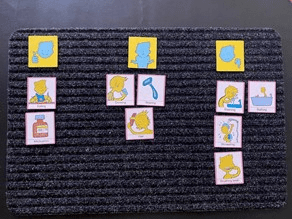
Picture 3 was during treatment for Psychosis and therapy – some changes were being noted with his self care and allowing his team to help him:
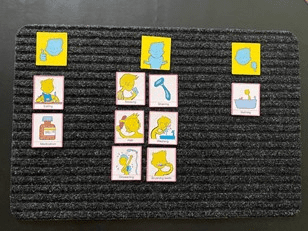
Picture 4 was towards the end of treatment and intensive therapy. Some aspects of bathing remained unsure, but his behaviour indicated that he was more comfortable with activities around bathing.
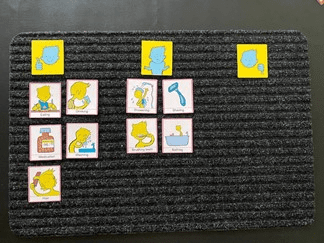
Picture 5 was a repeat of the family cards after treatment:
Picture 6 are the cards I have created based on the Mental State Examination – this was six months into therapy and medication. He expressed issues around his mood, thoughts and sleep – these needed more explaining. With the mood pictures, I offered my client different images for mood and he picked the ones that reflected what he was feeling. My mood collection has happy, angry, scared and sad in them as I tend to quote these 4 basic raw emotions daily in my work:
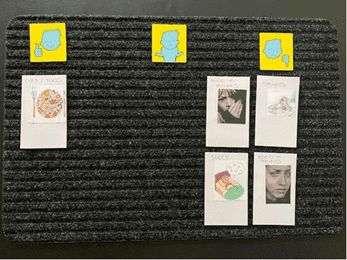
Picture 7 was at the end of treatment the same cards were used with a very different result. As for the previous mat, for the mood pictures, I offered my client different images for mood and he picked the ones that reflected what he was feeling:
Many thanks to Debbie Mole for sharing this powerful example. If you would like to read more about Talking Mats use in Mental Health, take a look at top 10 blogs here: https://www.talkingmats.com/top_10_mental_health/
If you are feeling inspired and have not yet accessed our Talking Mats Foundation Training Course, find out more here:
Many thanks to Karen Mellon, NHS Fife Lead Podiatrist for Learning Disabilities and Care Homes, for this guest blog describing our exciting Fife Health Charity funded project, aimed at supporting patients with a learning disability (LD), or dementia, to be more involved in decisions around their care.
I was initially introduced to Talking Mats by my Learning Disability SLT colleagues who were using the resource to support patient engagement. I could see the real benefits of how it could support our interactions with patients with a LD or dementia and empower people to be more involved with decisions around their care. Our SLT colleagues had undertaken the Talking Mats Train the Trainer program and were then able to train our podiatrists in using the resource. Having used the existing resources we found that we weren’t able to discuss/explore people’s views deeply enough, for example, when they developed a foot ulceration, or were at risk of ulceration. This was the spark that ignited the idea to look at developing a specific foot care resource to enable these conversations.
The aim was to promote patient engagement in their care – both in preventative care and when specialised input is required. By creating the resource we aimed to explore what really mattered to the person and what for them were acceptable goals and outcomes. By developing a specific Talking Mats resource we were able to explore treatments options and impact of conditions and actively engage the person in expressing their views thus creating a person centred care plan. Evidence shows us when people are involved in decision making they are more satisfied with their care, which in turns improves their quality of life.
Having consulted with Talking Mats we jointly created an initial resource which we piloted within NHS Fife over a 6 week period. People living within care homes and people with a learning disability were the target audience for the pilot. Using the resource, we were able to understand more about the impact that foot ulceration was having on patients, and patient’s views on treatment options.
One example of this positive impact involves a 60 year old patient with learning disabilities and dementia. She lives independently with one hour support each day to assist with personal care. She has been known to podiatry for some time due to repeated ulceration. Specialist footwear has been supplied and regular input is in place to reduce the risk of re-occurrence, however at times the foot does break down.
In May the patient experienced a break down on her foot. She is a very pleasant lady who always comes across as if nothing bothers her and everything is fine; she doesn’t like to “cause a fuss”. It was felt the use of a Talking Mat might give us greater insight into the impact the wound was having.
As a result of completing the Talking Mat we were able to discover the patient was in fact experiencing difficulties with the type of dressing and was experiencing pain. We were able to address this and change the dressing type to an adhesive dressing, which took up less room in her shoe, and started her on Paracetamol 4 times a day to address her pain. Follow up discussions reveal the patient was much more satisfied with the dressing, it was more comfortable and easier to keep dry when showering. She also reported to be experiencing much less pain.
As a result of the mat, we were able to identify concerns she had, but didn’t want to share as she didn’t want to be a burden. We were able to address this and create a plan which was acceptable to the patient and improved her wellbeing.
I hope this resource will go on to benefit other professionals and carers working with people who may be impacted by their foot health. By using this resource, we can help our patients explore their views and wishes, therefore enabling co-production in care. The resource promotes preventative care as well as specialist intervention. Going forward there are many other areas of foot health that could potentially be explored in developing further resources – such as paediatrics, nail surgery, musculoskeletal.
Book your place on the Talking Mats and foot care training course on 24th January 2024 / 21st February 2024 being run jointly between ourselves and Karen Mellon . The price includes the resource .
To find out more about the work and projects supported by the Fife Health Charity follow their Social Media accounts at:
Facebook – @fifehealthcharity
Twitter – @FifeHealth
The Talking Mats Foundation Training is a course that builds people’s confidence in using and applying Talking Mats to their work. Organisations can access this as a group ensuring staff can embed the Talking Mats approach and principles into their practice. The training also gives staff a common language for embedding a patient centred approach at the heart of a service.
We offer online training by;
- giving organisations access to our online training platform – this is designed as self-directed course, supported by a Talking Mats tutor, with a variety of activities and resources to support learning
- zoom/teams sessions
- a combination of both 1 and 2.
2020 saw an increase in organisations approaching Talking Mats for online team training and this has continued into 2021. We will work with you to find the approach that best suits your staff group.
Online learning does not suit everyone and comments from participants are mixed. Some really like the flexibility of being able to work at their own pace and find the site user friendly whilst others miss the interaction that face-to-face brings. As a team we miss the face-to-face training too but believe that our online training and the support we offer organisations is an excellent alternative.
It is easier to discuss the impact of an organisational course by giving an example. We recently ran a course using our online learning platform combined with short introductory and a follow-up session on Zoom for 24 staff working in an NHS Paediatric service. Taking part on the course were Nurses, Psychologists, Occupational Therapists, Physiotherapists, Dieticians and Speech and Language Therapists. It was great working with such a multidisciplinary group. They all have communication at the heart of their practice and were keen to learn about a framework that could help them improve the effectiveness of their work. There were different reasons for doing the course, but a common theme was wanting to have more ways of directly engaging and building relationships with the children they were working with rather than relying mostly on carer views. They wanted to be able to involve young people more meaningfully in some of the complex issues that surrounded their care.
It is always positive when a course has immediate impact and this staff group applied their learning in very different ways, for example Talking Mats was used to;
- communicate with a young person with selective mutism,
- involve a young woman who was self-harming to contribute to the strategies that help her reduce those behaviours ,
- involve children in physiotherapy interventions.
One course participant said ‘I have practised with a couple of patients and it has made a massive impact on their lives already. One patient’s behaviours have dramatically reduced as I was able to support her to show how she felt about aspects of her care and resolve this.’ And another participant said ‘I have now used Talking Mats with a couple of young people with complex neurodevelopmental difficulties and this has helped engagement considerably, where things had felt stuck before’
An important part of Talking Mats training is to help participants think about their own communication style and how it impacts on interactions and relationships. Staff said;
- this course increased my awareness of my communication style and made me reflect more on how I communicate with my patients but also what I presume from my patients.
- I am more aware of the communication demands I place on others as a clinician/therapist and am more confident in engaging people with communication difficulties.
- It has made me think more about the language that i use during interactions.
- It has definitely made me reflect on my own style of questioning, and helped improve my pacing and language skills.
The feedback from this varied and engaged group of staff was positive and is summed up in this comment; ‘The course was very engaging, interesting, and easy to follow and understand. I have learned a lot from this. The reflective work throughout the modules really helped to connect the theory with the practice of Talking Mats. The course leaders were very involved, supportive and helpful!’
Our training is relevant to organisations working within Social Work, Advocacy, Dementia Support and Education as well as Health and Social Care. If you think you would like to organise a course for your staff group please get in touch at info@talkingmats.com to talk it through.
Thanks to Kate Boot for the second part of her interesting blog describing her use of Talking Mats to assess and teach understanding of concepts and vocabulary related to Relationships and Sex Education, illustrating use of Talking Mats in a teaching context. Check out the first part of her blog here: https://www.talkingmats.com/sex-and-relationships-part-one/
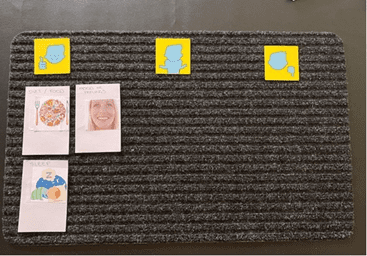
In the second part of this two-part blog series, I explore how using Talking Mats enables us to review the progress of linguistic and pragmatic understanding within the context of Relationships and Sex Education.
Considering the speech and language therapist’s focus is on increasing a person’s linguistic and pragmatic understanding we also use talking mats to explore potential target vocabulary and concepts. Drawing on the best evidence-based practice from the developmental literature (Steele and Mills, 2011; Justice et al, 2014; Lowe et al, 2018) we need to use a variety of methods to teach the underpinning vocabulary which wider RSE concepts relate to or hinge upon, e.g., safe, consent, power and control.
Using Talking Mats enables me to assess what the student already knows or understands of the vocabulary, which in turn informs the ongoing therapy programme, e.g., the degree of prompting or support needed to learn new words and to apply them to situational contexts. We repeat these activities throughout the academic year to evaluate how well the therapy programme is going and how the young adult’s understanding is developing.
Thinking back to Young Adult B from the first part of this blog, from their initial assessment, it was evident that they did not understand the word ‘safe’, therefore applying the evidence base described above we spent one term working on developing their understanding using a variety of communication friendly strategies. They even wrote two songs about the word ‘safe’ to the tune of Jingle Bells and Ariana Grande’s ‘Thank u, next’. Towards the end of the term, we completed a talking mat activity to review their progress. As I referred to in Part One it’s important to give control to the ‘thinker’, it is their mat.
Moving forwards, we will continue to review their progress using Talking Mats, which combined with the data from other best evidence-based practice will be used to determine the increase in their word knowledge which in turn, should develop their self-awareness and improve their skills needed to make decisions about sexual relations.
Kate Boot is Clinical Lead, Specialist Speech and Language Therapist and Sensory Integration Practitioner at Phoenix Learning and Care. To share ideas or chat further about this work you can contact her via Twitter @SLTinSEND or LinkedIn www.linkedin.com/in/kate-boot-salt
References
Justice, L. M., Schmitt, M. B., Murphy, K. A., Pratt, A., & Biancone, T. (2014). The ‘robustness’ of vocabulary intervention in the public schools: targets and techniques employed in speech–language therapy. International Journal of Language & Communication Disorders, 49(3), 288-303.
Lowe, H., Henry, L., Müller, L. M., & Joffe, V. L. (2018). Vocabulary intervention for adolescents with language disorder: a systematic review. International Journal of Language & Communication Disorders, 53(2), 199-217.
Steele, S. C., & Mills, M. T. (2011). Vocabulary intervention for school-age children with language impairment: A review of evidence and good practice. Child Language Teaching and Therapy, 27(3), 354-370.
Join the twitter chat exploring the recommendations of the Citizen’s Jury for people with intellectual disabilities and need for inclusive research practices In 2018 the Scottish Learning Disabilities Observatory and Talking Mats were funded by the Wellcome Trust to set up a Citizens’ Jury for people with learning/intellectual disabilities. We wanted to develop and test an adapted method of deliberative democracy, and hopefully to demonstrate that people with learning/intellectual disabilities can consider complex questions relating to health research. We also wanted to show that with resources, planning and good quality facilitation this could lead to valuable insights into inclusive research.
After a period of knowledge and skills development with our citizens’ jury members we held the jury over 5 days at the end of 2019. In early 2020 the Jury published their consensus report containing 10 recommendations for health research. You can watch a video the jury members made to communicate the recommendations here: Research Voices Citizens’ Jury: Our recommendations Involving People with Learning Disabilities – YouTube We believe that this report provides crucial insights into how people with learning/intellectual disabilities want to have their voices heard when it comes to health research. The next stage for us and the jury members is to secure further funding to build on this work and take forward the jury’s recommendations.
Through the Research Voices project we wanted to share our learning and develop resources that could be shared with the research community. Our evaluation report provides a detailed review of the Research Voices project with comprehensive information about the jury process and outcomes. There is an easy read version available.
On Tuesday the 8th of June we will host a twitter chat about inclusive health research from 7pm – 8p.m . We hope to welcome researchers, self-advocates, third sector organisations, carers and others to contribute to this discussion. If you have never joined a twitter chat before this is your opportunity. Here is how:
- At 7p.m on the 8th June go to twitter search on the hashtag #researchvoices.
- The first thing will be introductions – people can say who they are and where they come When you respond in a twitter chat always use the hashtag of the chat, in this case, #researchvoices. Using the hashtag allows everyone to see the conversation.
- Then we will post question 1 – when you respond to a question start with the question number e.g. Q1 but still remember to use the hashtag #researchvoices
- Later on question 2 and question 3 will be posted. To respond put Q2 or Q3 and the hashtag #researchvoices
- You can either respond directly to the questions or respond to the comments that other people have posed by saying what you liked or by asking them another question. Remember still use the hashtag #researchvoices in your response.
- Sometimes people just want to observe the conversation. That’s fine too but remember you can join in the conversation at anytime
- We look forward to seeing you on the 8th of June for this important twitter chat to share ideas and good practice
Questions….
Q1 How do the recommendations of the citizens Jury align with current research practice, what changes will you make to implement them, and what are the barriers to implementation?
Q2 What does successful inclusive practice look like to you – share your top tips for promoting inclusive research?
Q3 Inclusive research builds skills, expectations and connections with researchers with learning disabilities. Does the research community have responsibility for maintaining this long term and if so how?
In the UK we are emerging out of lockdown and there are concerns about the impact on the mental health of people at all ages and stages of life. This is a good time to reflect on the wide variety of blogs that have signposted how useful Talking Mats can be in helping people to think, structure coherent responses, and express their views. If this is an area of interest to you then take a look at these blogs to find out more:
- Edith Barrowcliffe from The Action Group demonstrates how Talking Mats has allowed individuals with intellectual disabilities access talking therapies and counselling. https://www.talkingmats.com/counselling-communication-1/
- Edith expands on this work in her second blog, describing how she adapted this approach to use during remote support during lockdown. https://www.talkingmats.com/counselling-learning-in-lockdown/
- Jo Brackley, NHS Clinical Lead for SLT Secure Services (Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust) describes how Talking Mats helps people with mental health open up and have richer conversations, with increased novel information gained. https://www.talkingmats.com/covid19_securehospitalsetting/
- Susan Gowland, SLT at NHS Fife Forensic Learning Disability Service, describes how Talking Mats support patients to express what they think in forensic learning disability setting. https://www.talkingmats.com/forensic_ld_setting/
- Dr Carla Innes, Clinical Psychologist for Learning Disabilities at Stockport Healthy Young Minds (CAMHS) describes how Talking Mats helps the team to gain more insight to the children and young people they are working with, and how it has helped intervention focus on the child’s potential, and zone of proximal development. https://www.talkingmats.com/talking-mats-and-mental-health/. This work in Stockport is further expanded on in a presentation by Dr Rosie Noyce, Clinical Psychologist, given at the Talking Mats 21st Birthday Event in August 2019. https://www.talkingmats.com/wp-content/uploads/2019/08/Talking-Mats-and-Young-Peoples-Mental-Health.pdf
- Georgia Bowker-Brady, Advanced Specialist SLT (Berkshire Healthcare Foundation Trust) describes how using Talking Mats in dementia care and acute health patient inpatient services helps patients organise their thoughts and express what is going well for them, as well as what isn’t. https://www.talkingmats.com/acute-mental-health/
- Rachel Woolcomb, Talking Mats OT Associate, explains why Talking Mats supports thinking, and why it can be particularly useful in helping people to structure and express their thoughts. https://www.talkingmats.com/talking-mats-as-a-thinking-tool/
We would love someone to carry out some research in this field, so if this sparks a research, or blog idea, please get in touch with us at info@talkingmats.com.
Many thanks to Peter Just, Head of External Affairs, RCSLT and Padraigin O’Flynn, External Affairs Assistant, RCSLT for this blog describing the newly launched UK-wide RCSLT Survey, which includes free Talking Mats resources to support those with communication difficulties to have their voices heard.
Like many of you, the Royal College of Speech and Language Therapists (RCSLT) has been worried about the impact of COVID-19 on people with communication and swallowing needs. Based on what we’ve heard from our members, service user organisations and service users themselves we’ve been very concerned about how the UK-wide lockdown (March-June 2020) affected people’s access to the speech and language therapy they and their families and carers need.
To help us understand the issue better and to inform our response, we’ve just launched a UK-wide survey. Following consultation with service user organisations, the three key questions we’re asking are:
- How did lockdown affect your speech and language therapy?
- What impact did this have on you?
- What are your thoughts about the future?
From the start, we were clear: we wanted the survey to be as accessible as possible to as many people as possible, no matter how they communicate and no matter what their communication preference is. Over the past couple of months, we’ve worked with members to produce the survey in a range of accessible formats.
We’re particularly delighted that one of those formats is Talking Mats – and we’re very grateful to Lois and Laura for all their advice and support . As you will know better than anyone, the mats will enable people to give us their views and tell us how they’ve felt and are feeling. We are delighted the mats will provide people with the means to self-advocate – this will add a richness to the survey findings that they might otherwise lack.
We’ll be working with service user organisations to promote the survey to their networks. But we’d also really like your help too. Please share the survey and encourage as many people as possible to fill it out. The more voices we hear, the more stories we collect and the more responses we receive, the greater the impact of the survey findings will be.
Those findings, which we hope to publish early in the New Year, will be used to influence Governments, Parliaments and Assemblies across the United Kingdom. The case that will be making to ministers, officials and parliamentarians – that people must have access to the speech and language therapy they need – will be all the stronger for it being based on service users’ lived experiences. The very powerful testimony that the mats will provide will strengthen that case even further.
The survey is open until 5pm on Friday, 8th January 2021 and you can find more information about it here:
https://www.rcslt.org/learning/has-coronavirus-affected-your-access-to-speech-and-language-therapy
We hope you find the mats useful and if you had any queries or wanted any more information, please let us know. We look forward to working with you to help make a difference to the lives of people with communication and swallowing needs.
Peter Just, Head of External Affairs, RCSLT
Padraigin O’Flynn External Affairs Assistant, RCSLT
Following on from last week’s guest blog, Edith Barrowcliffe from the Action Group describes how she has continued using Talking Mats throughout lockdown. Please note that the image used in this blog is from a mock session and has been taken for publicity purposes only.
In the second week of March I was running a 9 week old pilot counselling service (HearMe at The Action Group) for adults with cognitive and/or communication difficulties, supported by Talking Mats.
A week later lockdown catapulted me into remote working and demonstrated just how crucial Talking Mats were. Without access to the digital app or a suitably high resolution webcam my first online sessions were conducted without them. One client immediately began struggling to retain the thread of their subject matter.
I quickly rigged up a secondary webcam, allowing me to shift between my face and a clear view of the physical mat on my desk. Clients direct me how to place the symbols for them.
I’ve recently acquired a Talking Mats digital license and am pleased to find I can add in additional images. My experience with the physical cards is that allowing the client to direct the session often means searching through multiple different sets or hastily drawing new images. We move at a slower pace because of this but it seems to be an important way of giving weight and attention to whatever the client (Thinker) brings. My fantasy version of the digital talking mats app would include an image search function allowing me to rapidly search all the symbols in all the sets, pick one and caption it appropriately mid-session!
The client I mentioned above uses Talking Mats in this very freeform way – when they tell me something I ask if they want to put it on the mat and they will reply yes, or no. Once I’ve located or drawn the image they tell me where to place it. Towards the end of the session we review the mat, photograph it, and I send them the picture.
Another client uses a more structured approach. I present a choice of symbol sets based on topics that seem to be important to them (eg home environment, relationships, mobility). They select a topic and we begin a more typical talking mat, giving us a framework and focus to explore their feelings around each symbol. After a while the client/Thinker moves on to other emotionally weighted topics unrelated to the symbol set and we transition into something more akin to “regular” counselling – albeit with simplified, concrete, reflections of the kind proposed by Garry Prouty [1] Yet the Talking Mat seems to provide a “way in” to these deeper feelings that we otherwise don’t reach.
Not everyone uses Talking Mats. Lockdown has limited my capacity to offer it – not all clients have a computer/tablet for video calls and some clients actively prefer the phone. I’m continuing to learn, explore and find my way with this very diverse client group, but there is no doubt that Talking Mats opens up emotional exploration for some who might not normally manage it.
Edith Barrowcliffe, Hear Me, The Action Group
With thanks to our funders and partners for making this work possible – Hospital Saturday Fund, The Action Group Board, Leith Benevolent Society, Port o’Leith Housing Association, and The Scottish Government. And to the team at Talking Mats for their support and help!
[1] [PROUTY, G. (2008) Pre-Therapy and the Pre-Expressive Self. In: PROUTY, G. (ed.) Emerging Developments in Pre-Therapy. Monmouth: PCCS Books; also PÖRTNER, M. (2007) Trust and Understanding. Revised Ed. Ross-on-Wye: PCCS Books, pp82-85].
A new, updated version of our Digital app, will be available in the New Year. You can download a free taster version of our app here:
https://www.talkingmats.com/product/talking-mats-taster/
For more information about using Talking Mats remotely, check out this recent blog:
https://www.talkingmats.com/using-talking-mats-remotely/
 Online training login
Online training login