Many thanks to Mary Walsh, Health Service Executive (HSE) Senior SLT at St Mary’s Hospital, Dublin for this fantastic blog post about their project involving use of Talking Mats to support people with Dementia to participate in decision making related to their needs:
In September 2016 Aideen Lawlor (SLT Manager) and I (Senior SLT) won the Dementia Elevator award with a project entitled “Empowering Persons with Dementia to become more Active Participants in Decision Making Related to Their Present and Future Needs.” with Talking Mats being an integral part of this project. In November 2017, the prize money was used to fund my training to become an accredited Talking Mats trainer so that I could then train others in TM Foundation Course on a prioritised basis.
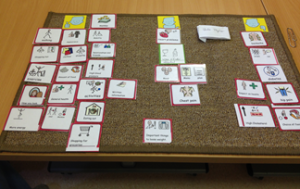
This project is now complete with 6 speech and language therapists (SLTs) from a variety of settings working with persons with dementia all trained in using Talking Mats. As part of their training, The SLTs used TM with patients/ residents with particular reference to the Assisted Decision Making (Capacity) Act 2015. TMs were also used to help the clinicians to get to know their patients, in care planning, in improving increased opportunities for interaction and in improving choices and decision making. In effect, we were checking it out!
All the SLTs found that when TM principles are followed, that it helped to empower people with dementia to make decisions about their care. Some of the reported findings:
- That the pictures help maintain attention and aid comprehension.
- That it facilitated strengths rather than a deficit model.
- That photographed completed TM provided a pictorial record for meetings – very positive.
- That it provided a significant catalyst for change in some instances.
- That it helped people with dementia and responsive behaviour get needs met
- That video recording sessions with consent greatly enhances reflective practice and may be helpful in key decision making
The next phase is to expand the number of SLTs who can provide training in Talking Mats across the Republic of Ireland. Funding from the national SLT professional body training grant scheme has been sought for these 6 SLTs to become trainers for Talking Mats. This will result in cascading training on a priority basis, increase evidence base/ knowledge re using TM and embedding TM in variety of clinical settings with SLTs leading this practice.
Mary Walsh,
Senior speech and language therapist,
St. Mary’s Hospital,
Phoenix Park, Dublin 20,
Ireland
Aideen Lawlor
Speech and Language Therapy Manager
If you are feeling inspired and are interested in accessing Talking Mats training, we offer Foundation Training courses throughout the UK and Ireland as well as online – take a look here for more details:
Once you have accessed Foundation Training you can apply for our Accredited Trainers course to enable you to deliver Talking Mats training to others in your area.
We are very grateful to Mary Walsh, Senior Speech and Language Therapist at St Mary’s Hospital in Dublin, for her Blog ;Does he like fairy cakes? ‘ It has been taken from her report on a project which looked at how speech and language therapists can facilitate the involvement of people with dementia to become more active participants in the decision making process around dysphagia management at the end stage of dementia. The project was funded by the Irish Hospice Foundation Changing Minds Programme
The project aims were:
- To improve person centred care in relation to residents’ food and drink preferences and dislikes
- To actively involve the residents of the dementia specific unit in the decision making process around their dysphagia (swallowing) management particularly at the end stage of their lives.
In order to find out the food and drink preferences and dislikes of the residents, the team carried out staff questionnaires and family questionnaires. They found that, although these were useful in getting a quick overview, there were a lot of unanswered questions.
The team also used Talking Mats and found it to be a powerful way to explore the residents’ food and drinks preferences and dislikes when used with suitable candidates. Participants appeared to really enjoy the experience including looking at pictures of the completed mats afterwards. This may be because they felt heard, that their views mattered and/or that they felt empowered. The information was important for current Dysphagia management, and also as an advanced directive in the documented evidence of the residents’ wishes in the recorded pictures of completed mats.
Brief Case Study: Does he like fairy cakes?
Talking Mats was used with a gentleman who may have been assumed to be unsuitable to use Talking Mats as he was assessed as having late stage dementia. However, this man engaged readily in the Talking Mats interview and appeared to be happy to have his views recorded. Also, there was a much higher level of correlation than variance with Talking Mats and both the staff questionnaire and the family questionnaire thus further indicating that he was a suitable candidate. ‘Fairy cakes’ was something that this resident reportedly liked in both the staff questionnaire and the family questionnaire. However, the gentleman indicated twice on Talking Mats that he disliked fairy cakes.
A number of actions are proposed in the report including :
- Continue to use Talking Mats as appropriate in the dementia specific residential unit and the rehabilitation wards of St. Mary’s Hospital.
- Inform the multi-disciplinary team of the merits of Talking Mats. This tool can also be used to explore other important issues for suitable residents/ patients on a case by case basis.
Conclusion:
It is essential to challenge our assumptions in our dealings with people with dementia. Truly person centred care takes time and patience where assumptions are challenged. Also, it is essential to listen to what residents tell us verbally, or through a supported communication system such as Talking Mats or non-verbally through tone of voice, facial expressions or gestures, and to act according to what is being communicated.
To read the full report please contact Mary Walsh at mary.walsh6@hse.ie To find out more about a Talking Mats resource that specifically focuses on finding out views on eating and drinking then please click here
Many thanks to Shirley Rush Health Facilitator at Belfast Health and Social Care Trust for this great blog about using TM as a ‘weigh to health’.
Following my Talking Mats (TM) training I had the opportunity, as a health facilitator, to use TM in an adapted ‘Weigh to Health’ course. This course encouraged people with learning disabilities to make small changes to their lifestyle and to educate them on the effects of obesity and their health.
Prior to commencing the group work we met with each person and completed a Talking Mat. The topic was to explore “Important things to lose weight”, we used a wide range of symbols and included physical activity, health conditions and appearance. Clients also requested additional symbols were added including alcohol, cycling and mood, which made the mat individual to them.
A photograph was taken of the completed TM to act as a record of what was important to them. On completion of the group the TM was repeated with each person using the same topic and symbols and the mat was again photographed. When we compared the TMs it showed that all the client’s knowledge and understanding of the effects of obesity and the health benefits associated with weight loss had increased.
“it done me good, helped me to lose weight by talking about my health and the need to lose weight to look after my heart”
The use of the talking mat was a valuable resource, it allowed each client to make an informed choice about participating in the group work. One client said he felt he had been listened too and “it done me good, helped me to lose weight by talking about my health and the need to lose weight to look after my heart”. By using TM in this way we have been able to use this information to demonstrate outcomes and it shows the information was presented at a level of understanding suitable for the client group. On an easy read questionnaire about the course all the clients agreed that doing the TM was useful, one person wrote “loved doing the mat”.
If you want to get more information from Shirley contact her at Shirley.rush@belfasttrust.hscni.ne
The Talking Mats Eating and Drinking resource provides insight into what service users perceive their difficulties to be and can help raise issues that care providers are unaware of.
Gillian Callander, speech and language therapist wrote the following review.
I have used this Talking Mats resource with adults with learning disability and it has been a valuable tool in discussing issues that they have with their eating and drinking and in providing a focus for discussion. It helps understanding of what can be an abstract and complex subject and can aid the planning of next steps.
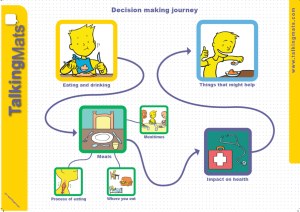
There are 3 symbol sets included with the resource
- Meals
- Health
- Things that might help
I have also used this resource with additional personalised symbols to discuss potential specific changes to eating and drinking and to gather information about how the service user would feel about this. There were blank symbols included with the resource which can be used for this purpose.
The symbols in this pack provide a range of subjects to be discussed and are clearly categorised. I have found that for the service users I work with that the “meals” set and “things that might help” have been the most relevant and easiest for discussion and the symbol sets provided ably support this. The “health” category is a little bit more abstract and is harder to discuss with this client group, particularly if this issue is one that may occur but currently is not causing any difficulties. However, it does provide a basis and support for this discussion and helps to tackle issues that are more complex and abstract.
I have found that using this Talking Mats resource has provided increased clarity during discussions with service users about eating and drinking and it provides service users with a more consistent method to express feelings about eating and drinking and the impact of any difficulties. It also supports me by giving a way to convey the information about concerns or potential changes to eating and drinking using the same method of communication as the service users, thus providing a method to enhance two way communication and facilitate discussions. It helps to ensure, that as far as possible, service users are able to input into the discussion about their eating and drinking and to make their opinions known. Using the Talking Mats has helped to provide evidence that service users do/do not understand the information being presented and can help decide outcome with regard to capacity for decision making.
Based on my experience of using this resource, I would recommend this as a valuable addition to your eating and drinking assessment tools.
Gillian Callander
We are holding a specialist Dysphagia and Decision Making training which includes the Eating & Drinking resource. Please follow this link to book your place
https://www.talkingmats.com/training/specialist-seminars/
Or download this flier and registration form: Dysphagia and Decision Making flier
What are the top 10 blogs for using Talking Mats with adults? Over the years we have posted lots of blogs on different aspects of our framework . If you are working with adults with communication disability these blogs maybe particularly helpful
- Where is the best place to start using the Talking Mats health and well-being resource?
- A blog from Denmark which highlights the effectiveness of using Talking Mats with people with dementia
- Goal setting with a woman with Multiple sclerosis
- Using the app with someone with aphasia
- The development of a resource to help people with learning disability raise concerns
- How can Talking Mats support Capacity to make decisions
- Involving people in their decisions about eating and drinking
- Thoughts on using Talking Mats with people with dementia to explore mealtimes
- Using Talking Mats with someone with a learning disability and dementia
- Use in a rehab setting in South Africa
If you want to explore our resource and training more please visit our shop
Following the success of previous seminars we are holding further specialist seminars in Stirling and London for anyone who has done the Talking Mats training. The topics will be:
- Talking Mats and the Eating and Drinking resource (morning)
- Talking Mats and Capacity (afternoon)
During the Eating and Drinking seminar, we provide background on how and why the resource was developed and showed some DVD examples of people using the resource. This really brings things to life and shows how important it is to give people (with and without speech) the opportunity to consider and talk about different aspects of eating and drinking. We also give people hands-on practice in using the symbols from each topic. Each participant will receive a copy of the full Eating and Drinking resource, including symbols, a mat, and explanatory booklet.
During the Capacity seminar we will discuss the fundamental principles of the Capacity Act and participants will have a chance to consider how Talking Mats can help people to:
- understand
- retain/remember
- weigh up information
- communicate their views/wishes and feelings.
They will also be given the opportunity to work through some practical examples and think about options to help people understand issues and make decisions.
If you have completed a Talking Mats training course and would like to attend either of specialist seminars, please click on the relevant course and fill in the registration form.
Stirling on Friday 29th April Stirling Seminars flier Apr 2016
London on Friday 10th June London Seminars flier June 2016
Registration form Seminar registration form 2016
One of the issues which has emerged from previous Talking Mats and dementia projects is that many people with dementia experience difficulties with mealtimes and that it can affect people at any stage of dementia.
Mealtimes involve two of our most fundamental human needs, the basic physiological requirements for food and drink and interpersonal involvement. Mealtimes are particularly important for people with dementia as they may develop difficulties both with eating as a source of nourishment and with the social aspects of mealtimes.
In 2015 Joan Murphy and James McKillop carried out a project, funded by the Miss EC Hendry Charitable Trust, to gather information from the first-hand experience of people with dementia about their views about mealtimes. We ran three focus groups and used the Talking Mats Eating and Drinking Resource to allow participants to reflect, express and share their views.
Findings:
The people who took part in this study felt that there were significant changes in their eating and drinking since their diagnosis of dementia. For some, their experience of mealtimes had changed and several said that they now skip breakfast and sometimes lunch. For some this seemed to be related to forgetting to eat and drink, for others it related to changes in taste whereas for others these meals seemed to be simply less important. Forgetting to eat was particularly noted by the participants with dementia and confirmed by their spouses.
The social aspect of eating and drinking also changed for many of the participants and, given the importance of social engagement for quality of life it is important to be aware of the effects of changes in eating and drinking on mealtime dynamics. For some it may be that they are now less interested in the social aspect of eating with others at home. Others found it hard to eat out because of distractions and lack of familiarity while some felt embarrassed about eating out in front of strangers. Others still really enjoyed going out for meals but added that they preferred to go somewhere well-known to them. The shared mealtime may be a particularly crucial opportunity for social engagement as it plays a central role in our daily lives. Social relationships are central for not only enhancing quality of life, but also for preventing ill health and decreasing mortality (Maher, 2013).
Almost all the participants talked about how their taste had changed both for food and drink which in turn affected their appetite. Some families had overcome the problem of lack of taste by going for more strongly flavoured food. When asked specifically about drinking, thirst was noted as a significant change since diagnosis
Their feelings about the texture of food did not appear to have changed significantly and was simply a matter of preference.
Three additional health issues which the participants felt were connected with eating and drinking were poorer energy levels than before their diagnosis, reduction in ability to concentrate and changes in sleep patterns.
For a copy of the full report please click here Dementia and Mealtimes – final report 2015
We are delighted to announce the release of Version 2 of the Talking Mats App
This app has a number of great new features which many of you have been asking for.
There are two new resources – Eating and Drinking – which has 3 main topic sets – Meals, Impact on Health and Things that might help.
There is an amazing new feature which many people have been asking for. Version 2 allows you to add your own images from your camera roll. This means that you can add you own personalised pictures to any of the topics.
Watch out for next week’s blog when Lois will tell you about her holiday using this new feature!
You can now also reset your password, use the Back button to navigate through the app, delete individual sessions and use the updated report page.
If you have already purchased the gold version of the Talking Mats app you will get all these new features for free.
If you wish to purchase the app please click here or for further information call our office 01786 479511
Recently we delivered two Talking Mats specialist seminars in London:
- Talking Mats and the Eating and Drinking resource
- Talking Mats and Capacity
Both seminars were very well attended with lots of discussion from a wide range of professionals.
During the Eating and Drinking seminar, we provided background on how and why the resource was developed and showed some DVD examples of people using the resource. This really brought things to life and showed how important it is to give people (with and without speech) the opportunity to consider and talk about different aspects of eating and drinking. We also gave people hands-on practice in using the symbols from each topic.
Each participant received a copy of the full resource, including symbols, a mat, and explanatory booklet.
During the Capacity seminar we discussed the fundamental principles the Capacity Act and participants had a chance to consider how Talking Mats can help people to:
- understand
- retain/remember
- weigh up information
- communicate their views/wishes and feelings.
They were also given the opportunity to work through some practical examples and think about options to help people understand issues and make decisions.
If you would like to attend our next specialist seminars, we are holding them in Stirling on 17th February: Stirling Seminars Feb 2015 flier
Whilst developing the eating and drinking resource, we tried it out with people with a range of eating and drinking difficulties. I talked to Ellie, who had swallowing difficulties following a stroke. She found it really helpful to use the mats to think about different aspects of meals (mealtimes, where you eat and the process of eating). Ellie had very good insight into her eating and drinking difficulties and had developed clear strategies to help manage them. She found breakfast and snacks the most difficult meals to manage. She was also very clear that pureed and soft moist foods were the safest and easiest for her. After we had done the mat, Ellie reflected on her eating and drinking, saying that it was limiting but that she could see that things had improved. One of the most difficult things for her was the impact of her swallowing difficulties on some of the social aspects of eating. She really misses going out for a meal with family and friends, something that we often take for granted.
Doing the ‘meals’ mat helped Ellie to see that although she still has many difficulties, mealtimes have become less stressful. For example, although eating and drinking is still a long, slow process, Ellie and her family have adapted to this and now manage ok, especially if they plan ahead. Some useful action points were also identified for the professionals working with Ellie – it would be good for her to have suggestions about a greater range of breakfast options as well as a variety of snacks which she could eat between meals.
Using the mats really helped to clarify the progress that Ellie has made with her eating and drinking since her stroke.
View the images used in the resource by downloading this short selection
To order your copy of the resource click here The resource will be available on our digital Talking Mat shortly
 Online training login
Online training login