The Talking Mats Board is delighted to appoint Dr Jill Bradshaw from the Tizard Centre, University of Kent, to the position of honorary research associate. This is our first appointment of this kind. Talking Mats is an evidence-based framework and research is important to us – but that research needs to be much more diverse, and involve a much wider range of people.
Jill’s role will be to give the Talking Mats team:
- A sounding board for research ideas and proposals
- Advice and support on publishing articles
- Identify research gaps and advise on funding avenues
We are also very aware that a number of people are using Talking Mats as a research tool, and Jill will also help to develop a virtual research network to bring interested researchers together. We are still exploring ways in which this could work, but it could involve an email network, virtual seminars and/or twitter chats. If you are interested in being included, and have completed our Talking Mats Foundation Training course, Jill would love to hear from you. Please email her on J.Bradshaw@kent.ac.uk – or email info@talkingmats.com and we will forward your interest to her.
Jill is really excited about this new post. She says ‘We know that the voices of people who have communication challenges can be excluded from research. This is a great opportunity to work with others to think about how we can use Talking Mats creatively in research and to find ways of including views from a wider range of people’.
Lois Cameron
November 2019
Talking Mats is now used in many countries all over the world. As part of our #TMis21 blog series, we wanted to share this great example of Talking Mats being used in Germany.
In March 2019 Prof. Dr. Norina Lauer (OTH Regensburg) and Elena Maxheimer held a lecture and a workshop about Talking Mats at the “aphasia days” in Wuerzburg, Germany. Many thanks to Norina and Elena for sharing information about the “aphasia days” for this blog post.
The “aphasia days” are a large congress – unique in Europe – for people with aphasia, family members and speech and language therapists (SLT). Every year around 600 people from Germany, Austria, Switzerland and Hungary are coming to this event. There are talks, workshops and podium discussions held by participants with aphasia, family members or SLTs. In front of approx. 150 listeners Norina and Elena gave a lecture about Talking Mats and the results of Elena’s bachelor thesis, in which she worked with people with aphasia, who learned to use Talking Mats.
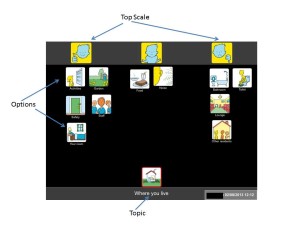
In a three-hour workshop at the “aphasia-days” Norina and Elena taught nine people with moderate to severe aphasia how to use Talking Mats. All persons brought their own tablets and logged into their own account. They where shown how to choose a topic and a top scale and practiced in teams of two. All of them conducted several sessions with different topics and switched partners a couple of times. They had a lot of fun talking about things that matter to them and learn more about their peers. At the end of the workshop they were able to use Talking Mats themselves and are going to use it with their relatives and friends at home. As the workshop was very well received by the participants, it is likely to be repeated at the next “aphasia days” 2020.
If you would like to find out more information about Talking Mats in Germany, and the Digital Talking Mats app which is now available in German, check out https://www.talkingmats.com/talking-mats-in-germany/ and https://www.talkingmats.com/german-digital-talking-mats-with-people-with-aphasia/
Our Talking Mats is 21 Event is in Stirling on Thursday 15th August 2019. Thanks to funding from NHS Forth Valley endowment committee the event is free but you do need to book your space https://www.eventbrite.co.uk/e/talking-mats-is-21-tickets-62362171935
You can come to the morning only, afternoon only or come for the whole day.
If you can’t come to our event watch out for out blogs and social media celebrating the reach of Talking Mats for 21 days before the 15th of August. Please join in with your contributions using the hashtag #TMis21. For 21 days after our event we will be having a special Birthday offer! Watch this space, more to follow …….
Talking Mats received funding from The Health and Social Care Alliance Scotland to look at how using the Digital Talking Mats can help people with long term conditions, including dementia, to manage their health and well-being and to recognise their own strengths and abilities. We also hoped that participants would be able to have more control over their lives and have improved communication with families and professionals.
11 people living with dementia and their partners were involved in the project. Each participant had a tablet device and was given a personal digital Talking Mats licence which gave them access to 13 topics in the Talking Mats Health and Well-being resource. We visited each participant at home, taught them how to use it and asked them to complete at least 1 digital Talking Mat per week for 6 weeks on any topic they wished. The design of the digital Talking Mat allowed them to email their mats directly to us. We visited each participant a second time to discuss how easy it was to use the digital Talking Mats and their views on their completed mats. We asked those who wished to, to continue sending us completed mats beyond the initial 6 weeks and we visited them again in 6 months to discuss how they were managing.
In total we received 94 digital mats across all 13 topics from the participants living with dementia who reported that the use of the Digital Talking Mats during this project gave them a better understanding of their own individual health and social care needs.
A woman with dementia said ‘It (Health mat ) made me realise things are not so bad and made me think I will continue with my exercise classes, carry on walking, socialising and eating well’
As well as helping participants self-manage their lives, an unexpected outcome of this project was that many people found that using the Digital Talking Mats helped them see the positive things in their life and not just the negative. It also highlighted that despite having a deteriorating illness, things were not getting worse.
‘This mat (Environment) showed me how happy I am in my own home and my neighbourhood’
The following are some of the comments we received throughout the project.
• It helps me sort out my thoughts – very useful
• I get so much out of the process
• I come up with insights which might help me in the future
• I can now talk to (my wife) in a way I couldn’t before
• I’m more relaxed now
• I come up with niggly health things that my partner didn’t know
‘It made me realise things are not so bad’.
If you know of anyone living with dementia would like to obtain the Digital Talking Mats please fill in the attached Personal Digital Licence 161117 DTM personal licence form with explanation and send it to us at info@talkingmats.com
This research will explore older father carers perspectives of caring for a son or daughter with learning disabilities. The aim of this project is to learn more about the experience of fathers who have a son or daughter with learning disabilities and how we can provide better supports and services for them in the future.
I am particularly interested in talking to fathers as mothers tend to be the focus when discussing the impact of caring on families who have a son or daughter with learning disabilities. While it is vital that we find out how to better support mothers, fathers’ role within the family and their experiences of caring are also very important. Despite this, fathers’ voices are rarely included in discussions about how service provision could be improved to meet these families’ needs.
The project focusses on older fathers (aged 60+) as I want to better understand the experiences of fathers who care for their son or daughter with learning disabilities over time. Fathers who are aged 60 and over will be able to talk about their experiences of caring at different times in their lives and how these experiences changed over time.
Fathers who participate in this project will attend an interview which lasts around one hour. I will meet fathers in their homes or at the University of Glasgow, depending on which option is more convenient for them. The interview involves discussing father’s experience of caring for their son or daughter with learning disabilities. We will discuss topics such as caring during their child’s early years, as they grew up, and more recently. We will talk about how the father’s relationship with their child and their caregiving role has changed over time, and how caring has impacted them.
If you think that you, or someone you know, would be interested in taking part in this project then please contact me at k.dunn.1@research.gla.ac.uk to find out more.
Self-management for people with long term conditions (LTC) is now a key government strategy to encourage people to take responsibility for their own health, behaviour and well-being. Talking Mats received funding from The Health and Social Care Alliance Scotland to look how using the Digital Talking Mats (DTM) can help people with LTCs to manage their health and well-being and to recognise their own strengths and abilities.
The overall aim of our project was to empower people with different long term conditions, to manage their own health and well-being. Through using Digital Talking Mats (DTM) we hoped that participants would be able to have more control over their lives and have improved communication with families and professionals.
There were a total of 28 participants in this project living with one of three different long term health conditions – stroke, dementia and learning disability. Each participant had access to a tablet device and was given a personal DTM licence which gave them access to 13 topics in the Talking Mats Health and Well-being resource. We visited each participant at home and taught them how to use it and asked them to complete and send us at least 1 digital mat per week for 6 weeks on any topic they wished. The design of the digital Talking Mat allowed them to email their mats directly to the researchers. We visited each participant a second time to discuss on how easy it was to use the digital Talking Mats and their views on their completed mats. We asked those who wished to, to continue sending us completed mats beyond the initial 6 weeks. We visited them again in 6 months to discuss how they were managing.
15 participants completed all 6 mats and 12 participants continued to complete mats over the length of the project. Participants completed 235 digital mats across all 13 topics
There were 3 particularly significant findings
1. At 18 months the participants living with dementia actually felt their well-being had improved, despite dementia being a progressive illness.
2. For the participants living with stroke the results were even more striking as 95% felt things were going well at the end of the project in comparison with 47% at the beginning.
3. At the end of the project the percentage of people with learning disability who felt things were not going well had reduced from 19% to 10%. Furthermore the percentage of people indicating that they were not sure about their views had increased from 27% to 42%. There can be a tendency for people with learning disability when using Talking Mats, to express their views at either end of the mat and to rarely use the mid- point. However being able to use the unsure mid- point is noteworthy as it indicates that the participants in the project realised that they could express their views not only as black or white but could indicate that they were unsure. This awareness opens up the potential for people to express views more thoughtfully with opportunities for further exploration.
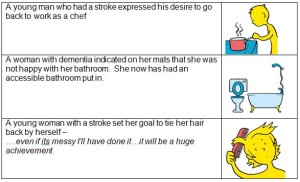
Here are three examples of how using the DTM supported people to self-manage situations in their lives. Click on image to enlarge.
As well as helping participants self-manage their long term conditions, an unexpected outcome of this project is that many people found that using the DTM helped them see the positive things in their life and not just the negative. It also highlighted that despite having a long term condition and, for many also a deteriorating one, that things were not getting worse.
Click here for full report including 6,12 and 18 month reports to the funders 20180717 Alliance full report
Click here for the summary report 20180717 Alliance Final Short Report
Click here for a video link of 2 participants
Talking Mats in Germany is being extended by one of our trainers Professor Norina Lauer. Here she describes two of her current interesting projects and we look forward to reading her findings.
The German version of the Talking Mats app will now be tested in two more projects in the west of Germany. As the communication symbols were developed for English-speaking clients six German SLT students of the Hogeschool van Arnhem en Nijmegen (han) in the Netherlands want to find out if the words and symbols fit to German clients and their cultural background. Because of cultural differences between Scotland and Germany it is necessary not only to adapt the language but also check the icons.
One of the projects will be conducted with children between the ages of 8 and 10 years. The children will be asked to classify the symbols from their age-group. The question will be whether the symbols and words are relevant for the situation of German children. If not, they will be asked for possible alternatives.
The other project focuses on adults. One group of people with aphasia and one group of healthy persons will be tested. Every tested person scores the 57 icons concerning their correspondence with the words written down below by using a scale from 0 to 3. In addition, possible graphic alternatives will be enquired and collected. The two groups of adults will be used to determine if there is a significant difference between the obtained results from each group.
Apart from the necessity of fulfilling the requirements of the General Data Protection Regulation which has to be completed by 25th May, I have been pondering on other advantages of complying with the GDPR.
Here at Talking Mats we are all going through files, bagging up paper for shredding, deleting data files on our master computer and preparing text to send to all our customers and contacts to make sure we only hold information that is adequate and relevant.The first advantage for us is that it’s a good way to re-establish contact with people.
I’ve been given the task of going through all the research data and have ploughed through 16 drawers of research data starting in 1992! Way back then I worked with a wonderful professor who was keen to hold onto all our raw data just in case we wanted to check or replicate anything. Its all been under lock and key but the time has come to bite the bullet and get rid of it. I found this to be not only nostalgic but also emotional – all those fantastic participants who gave us their time and insights.
Its also been cathartic because as well as filling bags for shredding I am smashing up discs of video footage. We filmed lots of people with a range of communication difficulties using Talking Mats to compare with the same conversations without Talking Mats to analyse any differences. So… another big advantage is that I’ve destroyed all evidence of my dodgy hair cuts throughout the years!!
I counted 41 completed projects going from the very first one in 1992 which was a demographic survey of people who used AAC (Augmentative and Alternative Communication) systems in Scotland. In 1998 the Gannochy Trust funded the original project where Talking Mats was born Gannoch Final report. We then went on to carry out a wide range of projects which include working with people with Motor Neuron Disease, Stroke, Learning Disability, Children with Additional Support Needs, people living with Dementia to name but a few. The website contains the final reports on all our projects and in looking back at them I am also very proud of the good quality research the team here at Talking Mats has carried out.
Many others are now doing projects using Talking Mats but I leave it to them to organise their own GDPR and hope they also find the process worthwhile and rewarding and not just seen as a chore to be done.
Five short stories from our recent accredited training course in Stirling.
- A looked after child was unhappy but no one knew specifically why. Using the Talking Mats, she indicated that she was upset by the weekly phone call with her mother because it always happened when it was her playing time. The time of the call was moved to just before her bedtime but this resulted in bad dreams. The time of the call was finally moved to Saturday afternoon which helped her settle and reduced her distress.
- Talking Mats was used with an Iraqi boy who had come to England via Libya, Italy and the jungle camp at Calais. When he picked the symbol of a waiting room he indicated that despite all she had been through he really liked this because it reminded him of all the children in his family and made him happy.
- A 76-year-old man with a learning disability disclosed that he had been attacked and suffocated by his upstairs neighbour one week previously. It was only when he used the Talking Mats that he disclosed to anyone what had happened.
- A lecturer usually used quantifying measuring with her students to find out how they were managing their studies. Instead she used Talking Mats to find out how they were coping with their work life balance. One student told her that she was managing fine except that her pet rabbits always escape under the bed and it takes her a long time to get them back out so she does not let them out very often!
- Talking Mats was used with a man who had had a stroke and had to go into residential care because his family could no longer look after him. They were very worried that he was unhappy with the new care set up. He was able to show with the Talking Mats that he was happy about everything except that he was not given enough time when he went to the toilet. Once the staff realised this they then gave him more time which resolved the situation and reassured his family.
Please send us your Talking Mats stories – we love hearing them.
We are delighted to have Celine Josephine Giese, a 4th year psychology student from the University of Stirling, on placement with us. As part of her placement she has to write a series of blogs which she has kindly shared with us. This is the first in the series.
Talking Mats is a social enterprise, that has developed a unique communication system that aspires to improve quality of life for people who struggle to communicate effectively, such as people with a learning disability or a stroke as well as people who have dementia. People who are affected by communication barriers have difficulty articulating their needs, emotions and wishes, which can be particularly challenging for carers and clinical practitioners.
The interactive communication tool consists of an actual doormat and different sets of communication symbols that are placed on the Talking Mat. The communication symbols represent a scale from positive, medium to negative. Specifically, designed topical image sets are used to communicate how the person feels about activities, eating, support and so forth. In addition, they also developed a digital app version.Talking Mats simplifies the communication process by breaking down information into small manageable chunks without the need for literacy. A range of training courses are offered to help individuals to use Talking Mats effectively.
The first day I arrived I was excited as I have not worked in an office environment before. In advance of the meeting I read a lot about their concept and ongoing projects to demonstrate my enthusiasm and interest. I was introduced to the team, who were all very kind and welcoming. During the first meeting, I was introduced to their communication system via a Talking Mat with a general interests’ topic to get to know me better. This was a great way to understand and see how their system works in action. We also filled out the placement agreement and discussed the project I will be involved in.
My role involves supporting Talking Mats in the analysis and impact of the training. For this I am looking at recorded Talking Mat outcome stories from trainees as part of a large-scale project in London Health Authority. I am recording specific details of the stories in an excel spreadsheet, such as the outcome for the patients which will aid the further development of Talking Mats and give feedback to the funders on their investment. Moreover, this analysis will shed light on the bigger impact Talking Mats has on the communication between patients and their carers.
The analysis will be useful in determining the impact Talking mat has on the person whose mat it is and on who used the mat i.e. the interviewer. In addition, it will provide evidence to the organisation of the effectiveness of using Talking Mats. My involvement in the thematic analysis will allow me to further develop excel skills and experience an office setting in a social enterprise, while expanding my knowledge on its origins, current use and future direction potential. Because the cases disclose patients’ personal details I have signed a confidentiality agreement. I look forward to learning more and contributing to the project as well as working with the team. The atmosphere is both pleasant and inspirational and I admire the concept of the enterprise and I feel privileged to be part of such a life changing organisation.Celine’s second blog will be posted soon.
We are very grateful to Lauren Pettit and her colleagues from Pretoria, South Africa for sending us their published paper on a recent research project which used Talking Mats as a research method.
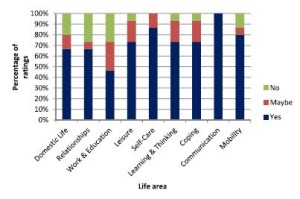
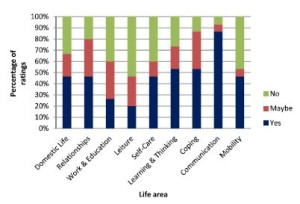
The study’s aim was to describe and compare the views of adults with aphasia, their significant others and their speech and language pathologists regarding the importance of nine life areas for the rehabilitation of adults with aphasia.
They used Talking Mats to support 15 adults with expressive aphasia to rate 9 life areas in terms of importance to them. The 9 life areas they included were Domestic Life, Relationships, Work and Education, Leisure, Self-care, Learning and Thinking, Coping, Communication and Mobility. These are taken from the World Health Organisation International Classification of Functioning Disability and Health (WHO-ICF). The researchers also obtained the ratings of 15 significant others and the 15 speech and language pathologists treating them.
They found that most life areas were rated as important to work on in rehabilitation by most participants. However, there were some discrepancies between the views of the adults with aphasia and the other 2 groups in the study and significant discrepancies were noted for 3 of the 9 life areas.
The graphs below show the comparisons of the 3 groups of participants. Click on graphs to enlarge
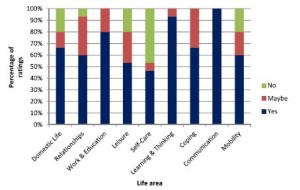
The researchers suggest that ‘These life areas can provide the ‘common language’ for team members to engage in dialogue and identify problem areas related to the daily life functioning of people with expressive aphasia. By simplifying some of the labels of the activities and participation dimensions of the WHO-ICF and pairing these labels with pictures and the interactive Talking Mats interview procedure, adults with expressive aphasia (who often have difficulty participating in the selection of rehabilitation priorities) were able to express their own views. This may be a first step in assisting the adult with aphasia to advocate for themselves and to exercise their right to identify the activities and participation opportunities which they would like to access, and to set rehabilitation priorities based on their choice. While the overlap in priorities among the three groups as found in this study is encouraging, the presence of some significant differences underlines the importance of the voice of adults with aphasia themselves. This ensures truly client-centred rehabilitation that underscores the principles of human rights and a focus on competence rather than deficits’.
To link to the full article: http://dx.doi.org/10.1080/10749357.2016.1207148aphasia
Please contact info@talkingmats if you would like to discuss using Talking Mats in research
 Online training login
Online training login